The relationship between tinnitus characteristics, stress and depression in patients with subjective tinnitus
Main Article Content
Abstract
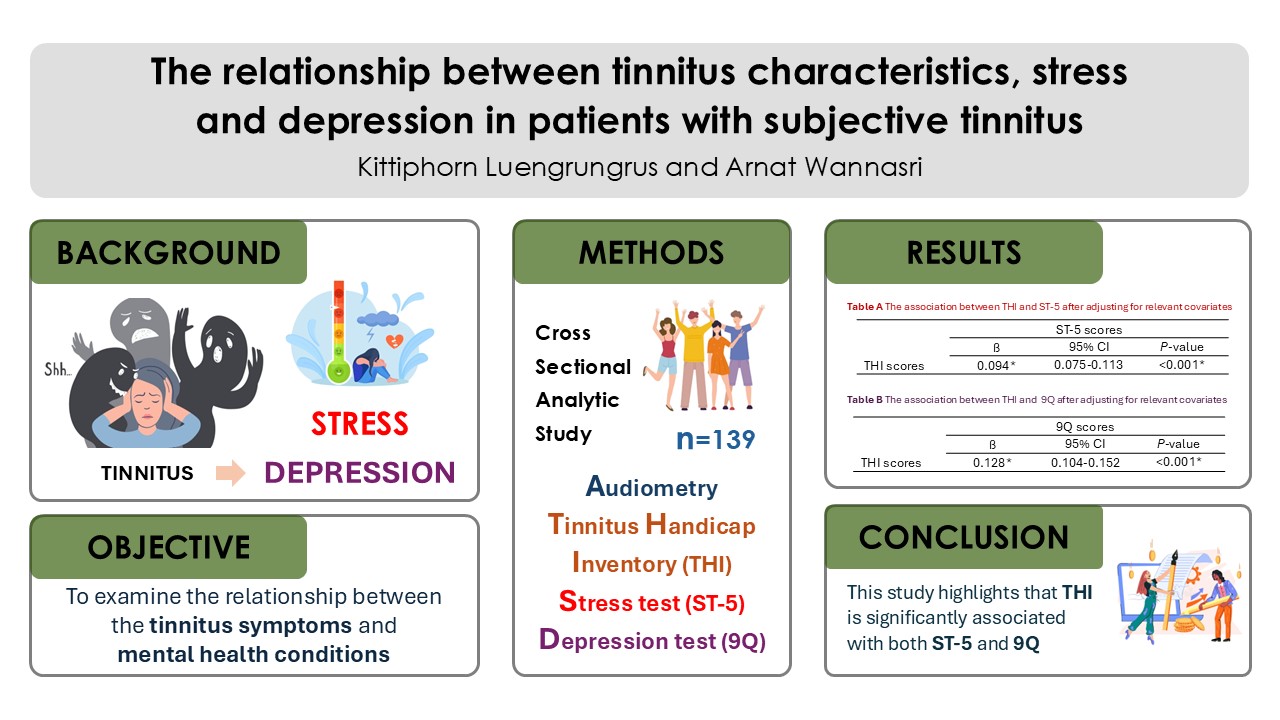
Background: Tinnitus is a perception of a noise in the ears. Individuals with tinnitus symptoms may experience disrupt daily life activities and mental health issues such as stress and depression.
Objectives: This study aimed to examine the relationship between the tinnitus symptoms and mental health conditions – stress and depression – in individuals with subjective tinnitus.
Materials and methods: This was an analytical cross-sectional study, involved 139 participants with subjective tinnitus aged between 18 and 70 years. All participants underwent clinical hearing tests. The tinnitus severity level was assessed by the Tinnitus Handicap Inventory in Thai version (THI), while the Stress Test 5 (ST-5) and the nine-question depression screening test (9Q) were used to assess stress and depression, respectively.
Results: After adjusting for tinnitus-related variables, the overall THI scores showed significantly positively associated with both the ST-5 and 9Q scores. Additionally, gender was also significantly positively associated with the 9Q scores. In contrast, other tinnitus-related factors including age, affected ear, tinnitus pattern and duration and average hearing thresholds in the affected ear, showed no statistically significant correlations with the ST-5 and 9Q scores.
Conclusion: This study highlights a significant association between the THI scores and both ST-5 and 9Q, indicating that tinnitus severity is closely linked to the development of stress and depression. Therefore, it is essential to monitor and manage psychological distress in patients with tinnitus.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Ty ler RS, Noble W, Coelho C, Roncancio ER, Jun HJ. Tinnitus and hyperacusis. In: Katz J, editor. Handbook of clinical audiology. 7th Ed. Philadelphia: Wolters Kluwer Health; 2015. p. 647-72.
McCormack A, Edmondson-Jones M, Somerset S, Hall D. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res. 2016; 337: 70-9. doi: 10.1016/j.heares.2016.05.009.
Hackenberg B, Döge J, O’Brien K, Bohnert A, Lackner KJ, Beutel ME, et al. Tinnitus and its relation to depression, anxiety, and stress—a population-based cohort study. J Clin Med. 2023; 12(3): 1169. doi: 10.3390/jcm12031169.
Scheffer AR, Mondelli MFCG. Tinnitus and hearing survey: cultural adaptation to Brazilian Portuguese. Braz J Otorhinolaryngol. 2021; 87(1): 28-34. doi: 10.1016/j.bjorl.2019.06.009.
Ciminelli P, Machado S, Palmeira M, Carta MG, Beirith SC, Nigri ML, et al. Tinnitus: The sound of stress? Clin Pract Epidemiol Ment Health. 2018; 14(1): 264-9. doi: 10.2174/1745017901814010264.
Musleh A, Alharthy AKH, Alzahrani MYM, Bin Maadhah SA, Al Zehefa IA, AlQahtani RY, et al. Psychological impact and quality of life in adults with tinnitus: A cross-sectional study. Cureus. 2024; 16(1): e51976. doi: 10.7759/cureus.51976.
Zöger S, Svedlund J, Holgers KM. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics. 2006; 47(4): 282-8. doi: 10.1176/appi.psy.47.4.282.
Zhang L, Du H, You H. Correlation between the degree of hearing loss and the levels of anxiety and depression in patients with tinnitus. Noise Health. 2023; 25(118): 195-201. doi: 10.4103/nah. nah_46_23.
Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER, et al. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg. 2014; 151(2 Suppl): S1-40. doi: 10.1177/019 4599814545325.
Department of Otolaryngology, Nopparat Rajathanee Hospital. Outpatient statistics of patients receiving hearing examinations, Fiscal year 2024. Bangkok: Nopparat Rajathanee Hospital; 2024. (in Thai).
Limviriyakul S, Supavanich W. The validity and reliability of tinnitus handicap inventory Thai version. J Med Assoc Thai [Internet]. 2012; 95(11): 1433-40. Available from: https://pubmed.ncbi.nlm.nih.gov/ 23252210/.
Department of Mental Health, Thailand. Stress Test-5 (ST-5) [Internet]. 2019 [cited 2024 May 12]. Available from: https://dmh.go.th/test/Download/view.asp?id=18.
Department of Mental Health, Thailand. 9-Question Depression Screening Test (9Q) [Internet]. 2019 [cited 2024 May 12]. Available from: https://dmh.go.th/test/Download/view.asp?id=22.
Kim SY, Jeon YJ, Lee JY, Kim YH. Characteristics of tinnitus in adolescents and association with psychoemotional factors. Laryngoscope. 2017; 127(9): 2113-9. doi: 10.1002/lary.26334.
Hébert S, Lupien SJ. The sound of stress: Blunted cortisol reactivity to psychosocial stress in tinnitus sufferers. Neurosci Lett. 2007; 411(2): 138-42. doi: 10.1016/j.neulet.2006.10.028.
Lee JH, Ra JJ, Kim YH. Adequacy of the simplified version of the Tinnitus Handicap Inventory (THI-S) to measure tinnitus handicap and relevant distress. Korean J Audiol. 2014; 18(1): 19-27. doi: 10.7874/kja.2014.18.1.19.
Murtaza M, Saqulain G, Rao RA. Characteristics of tinnitus and its association with clinicodemographic factors and mental health. J Riphah Coll Rehabil Sci. 2024; 12(1): 3-9. doi: 10.53389/JRCRS.2024120102.
Ratnayake SAB, Jayarajan V, Bartlett J. Could an underlying hearing loss be a significant factor in the handicap caused by tinnitus? Noise Health. 2009; 11(44): 156-60. doi: 10.4103/1463-1741.53362.
Wang Y, Zhang JN, Hu W, Li JJ, Zhou JX, Zhang JP, et al. The characteristics of cognitive impairment in subjective chronic tinnitus. Brain Behav. 2018; 8(3): e00918. doi: 10.1002/brb3.918.
Waechter S. Association between hearing status and tinnitus distress. Acta Otolaryngol. 2021; 141(4): 381-5. doi: 10.1080/00016489.2021.
Aazh H, Salvi R. The Relationship between severity of hearing loss and subjective tinnitus loudness among patients seen in a specialist tinnitus and hyperacusis therapy clinic in UK. J Am Acad Audiol. 2019; 30(8): 712-9. doi: 10.3766/jaaa.17144.
Khilnani AK, Thaddanee R, Chodvadiya M, Khilnani G. Correlation of severity of tinnitus with severity of anxiety and depression in adults in a tertiary care hospital at Bhuj, Gujarat, India. Int J Otorhinolaryngol Head Neck Surg. 2018; 4(4): 1044. doi: 10.18203/issn.2454-5929.ijohns20182710.
Meijers SM, Lieftink AF, Stegeman I, Smit AL. Coping in chronic tinnitus patients. Front Neurol. 2020; 11: 570989. doi: 10.3389/fneur.2020.570989.
Meijers SM, Rademaker M, Meijers RL, Stegeman I, Smit AL. Correlation between chronic tinnitus distress and symptoms of depression: A systematic review. Front Neurol. 2022; 13: 870433. doi: 10.3389/fneur.2022.870433.
Zeman F, Koller M, Langguth B, Landgrebe M, Figueiredo R, Aazevedo A, et al. Which tinnitusrelated aspects are relevant for quality of life and depression: results from a large international multicentre sample. Health Qual Life Outcomes. 2014; 12(1): 7. doi: 10.1186/1477-7525-12-7.
Xu Y, Yao J, Zhang Z, Wang W. Association between sleep quality and psychiatric disorders in patients with subjective tinnitus in China. Eur Arch Oto-Rhino-Laryngology. 2016; 273(10): 3063-72. doi: 10.1007/s00405-016-3906-8.
Weidt S, Delsignore A, Meyer M, Rufer M, Peter N, Drabe N, et al. Which tinnitus-related characteristics affect current health-related quality of life and depression? A cross-sectional cohort study. Psychiatry Res. 2016; 237: 114-21. doi: 10.1016/j.psychres.2016. 01.065.
Lockwood AH, Salvi RJ, Coad ML, Towsley ML, Wack DS, Murphy BW. The functional neuroanatomy of tinnitus: Evidence for limbic system links and neural plasticity. Neurology. 1998; 50(1): 114–20. doi: 10.1212/ wnl.50.1.114.
Yehuda R, Boisoneau D, Mason JW, Giller EL. Glucocorticoid receptor number and cortisol excretion in mood, anxiety, and psychotic disorders. Biol Psychiatry. 1993; 34(1-2): 18-25. doi: 10.1016/ 0006-3223(93)90252-9.
Lee SS, Han K Do, Joo YH. Association of perceived tinnitus with duration of hormone replacement therapy in Korean postmenopausal women: a cross-sectional study. BMJ Open. 2017; 7(7):e013736. doi: 10.1136/bmjopen-2016-013736.
Han TS, Jeong JE, Park SN, Kim JJ. Gender differences affecting psychiatric distress and tinnitus severity. Clin Psychopharmacol Neurosci. 2019; 17(1): 113-20. doi: 10.9758/cpn.2019.17.1.113.
Gomaa MAM, Elmagd MHA, Elbadry MM, Kader RMA. Depression, Anxiety and Stress Scale in patients with tinnitus and hearing loss. Eur Arch Otorhinolaryngol. 2014; 271(8): 2177-84. doi: 10.1007/s00405-013-2715-6.
Malakouti SK, Nojomi M, Mahmoudian S, Alifattahi N, Salehi M. Comorbidity of chronic tinnitus and mental disorders. Int Tinnitus J [Internet]. 2011; 16(2): 118-22. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22249870.
Niemann U, Brueggemann P, Boecking B, Mazurek B, Spiliopoulou M. Development and internal validation of a depression severity prediction model for tinnitus patients based on questionnaire responses and socio-demographics. Sci Rep. 2020; 10(1): 4664. doi: 10.1038/s41598-020-61593-z.