Prevalence and associated factors of pre-frailty and frailty among Thai community-dwelling older adults aged 65 years and above
Main Article Content
Abstract
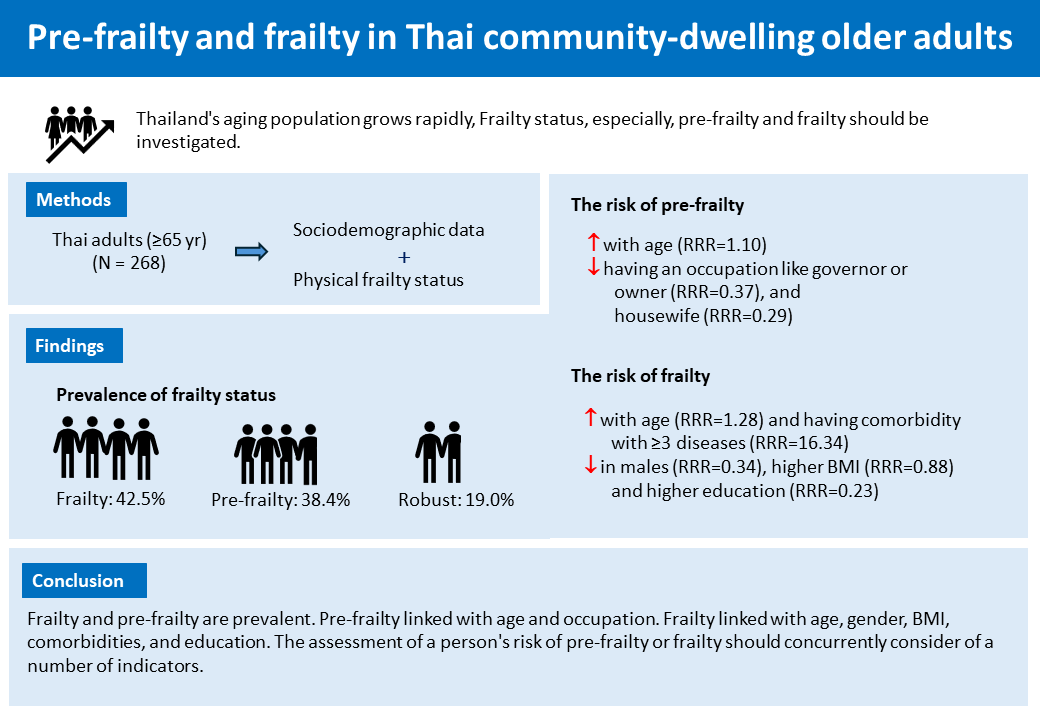
Background: As Thailand’s aging population grows rapidly, frailty status may develop and have serious implications. Early detection or prevention can be encouraged, especially prior to the emergence of advanced frailty and functional deterioration. Pre-frailty and frailty should be identified and investigated.
Objectives: To explore the prevalence of frailty statuses and their associations with sociodemographic characteristics among Thai older adults.
Materials and methods: This study was a cross-sectional design. Two hundred sixty-eight Thai community-dwelling older adults aged ≥65 years were recruited. Their physical frailty status was determined using the Fried frailty phenotypic criteria, which comprise weakness, slowness, low physical activity, weight loss, and exhaustion. Multinomial (Polytomous) logistic regression was used to detect associations between frailty status and sociodemographics.
Results: Among participants, the prevalences of pre-frailty, frailty, and robustness were 38.4%, 42.5%, and 19.0%, respectively. In the multivariate-adjusted model, pre-frailty was significantly associated with age (relative risk ratio(RRR)=1.10; 95% confidence interval (CI)=1.01-1.18, p=0.020), occupation as governor or owner (RRR=0.37; 95%CI=0.15-0.92, p=0.032), and housewife (RRR=0.29; 95%CI=0.09-0.93, p=0.037). Likewise, frailty was associated with age (RRR=1.28; 95%CI=1.18-1.39, p<0.001), gender (RRR=0.34; 95%CI=0.14-0.85, p=0.021), BMI (RRR=0.88; 95%CI=0.79-0.98, p=0.019), and education (RRR=0.23l; 95%CI=0.09-0.58, p=0.002). Additionally, comorbidity with ≥3 diseases was significantly associated with frailty (RRR=16.34; 95%CI=1.64-162.46, p=0.017).
Conclusion: Our findings reveal comparable prevalence rates of pre-frailty and frailty among Thai older adults. While age and occupation were associated with pre-frailty, a broader range of factors, including age, gender, BMI, comorbidities, and education, showed associations with frailty. These results underscore the importance of considering multiple factors collectively when screening or assessing an elderly individual’s risk of developing pre-frailty or frailty.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Sezgin D, Liew A, O’Donovan MR, O’Caoimh R. Pre-frailty as a multi-dimensional construct: a systematic review of definitions in the scientific literature. Geriatr Nurs. 2020; 41(2): 139-46. doi: 10.1016/j.gerinurse.2019.08.004.
Fernández-Garrido J, Ruiz-Ros V, Buigues C, Navarro-Martinez R, Cauli O. Clinical features of prefrail older individuals and emerging peripheral biomarkers: a systematic review. Arch Gerontol Geriatr. 2014; 59(1): 7-17. doi: 10.1016/j.archger.2014.02.008.
O’Caoimh R, Sezgin D, O’Donovan MR, Molloy DW, Clegg A, Rockwood K, et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing. 2021; 50(1): 96-104. doi: 10.1093/ageing/afaa219.
Zeng XZ, Meng LB, Li YY, Jia N, Shi J, Zhang C, et al. Prevalence and factors associated with frailty and pre-frailty in the older adults in China: a nation-al cross-sectional study. Front Public Health. 2023; 11: 1110648. Published 2023 Jul 24. doi: 10.3389/fpubh.2023.1110648.
Shimada H, Makizako H, Doi T, Tsutsumimoto K, Suzuki T. Incidence of disability in frail older persons with or without slow walking speed. J Am Med Dir Assoc. 2015; 16(8): 690-6. doi: 10.1016/j.jamda.2015.03.019.
Rodríguez-Laso Á, García-García FJ, Rodríguez-Mañas L. Transitions between frailty states and its predictors in a cohort of community-dwelling Spaniards. J Am Med Dir Assoc. 2022; 23(3): 524.e1-e11. doi: 10.1016/j.jamda.2021.07.008.
Wongtrakulruang P, Muangpaisan W, Panpradup B, Tawatwattananun A, Siribamrungwong M, Tomongkon S. The prevalence of cognitive frailty and pre-frailty among older people in Bangkok metropolitan area: a multicenter study of hospital-based outpatient clinics. J Frailty Sarcopenia Falls. 2020; 5(3): 62-71. doi: 10.22540/JFSF-05-062.
Thinuan P, Siviroj P, Lerttrakarnnon P, Lorga T. Prevalence and potential predictors of frailty among community-dwelling older persons in Northern Thailand: a cross-sectional study. Int J Environ Res Public Health. 2020; 17(11): 4077. doi:10.3390/ijerph17114077.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001; 56(3): M146-56. doi: 10.1093/gerona/56.3.m146.
O’Caoimh R, Galluzzo L, Rodríguez-Laso Á, Van der Heyden J, Ranhoff AH, Carcaillon-Bentata L, et al. Transitions and trajectories in frailty states over time: a systematic review of the European Joint Action ADVANTAGE. Ann Ist Super Sanita. 2018; 54(3): 246-52. doi: 10.4415/ANN_18_03_12.
Sergi G, Veronese N, Fontana L, De Rui M, Bolzetta F, Zambon S, et al. Pre-frailty and risk of cardiovascular disease in elderly men and women: the Pro.V.A.study. J Am Coll Cardiol. 2015; 65(10): 976-83. doi: 10. 1016/j.jacc.2014.12.040.
Rattanawiwatpong P, Khunphasee A, Pongurgsorn C, Intarakamhang P. Validity and reliability of the Thai version of short format international physical activity questionnaire (IPAQ). J Thai Rehabil. 2006; 16: 147-60.
Orme JG, Reis J, Herz EJ. Factorial and discriminant validity of the center for epidemiological studies depression (CES-D) scale. J Clin Psychol. 1986; 42: 28-33. doi: 10.1002/1097-4679(198601)42:1<28::aid-jclp2270420104>3.0.co;2-t.
Zhang Z. Model building strategy for logistic regression: purposeful selection. Ann Transl Med. 2016; 4(6): 111. doi: 10.21037/atm.2016.02.15.
Gordon SJ, Baker N, Kidd M, Maeder A, Grimmer KA. Pre-frailty factors in community-dwelling 40-75 year olds: opportunities for successful ageing. BMC Geriatr. 2020; 20(1): 96. doi: 10.1186/s12877-020-1490-7.
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012; 60(8): 1487-92. doi: 10.1111/j.1532-5415.2012.04054.x.
Shinohara T, Saida K, Tanaka S, Murayama A, Higuchi D. Transition to frailty in older Japanese people during the coronavirus disease 2019 pandemic: a prospective cohort study. Arch Gerontol Geriatr. 2022; 98: 104562. doi: 10.1016/j.archger.2021.104562.
Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011; 27(1): 1-15. doi: 10.1016/j.cger.2010.08.009.
Morley JE. Frailty and sarcopenia in elderly. Wien Klin Wochenschr. 2016; 128(Suppl 7): 439-45. doi: 10.1007/s00508-016-1087-5.
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011; 305(1): 50-8. doi: 10.1001/jama.2010.1923.
Castell MV, Sánchez M, Julián R, Queipo R, Martín S, Otero Á. Frailty prevalence and slow walking speed in persons age 65 and older: implications for primary care. BMC Fam Pract. 2013; 14: 86. doi: 10.1186/1471-2296-14-86.
Norheim KL, Bøggild H, Andersen JH, Omland Ø, Bønløkke JH, Madeleine P. Retirement status and frailty: a cross-sectional study of the phenotype of manual workers aged 50-70 years. Eur J Public Health. 2021; 31(1): 116-21. doi: 10.1093/eurpub/ckaa188.
Yoshizawa Y, Tanaka T, Takahashi K, Fujisaki-Sueda-Sakai M, Son BK, Iijima K. Impact of health literacy on the progression of frailty after 4 years among community-dwelling older adults. Int J Environ Res Public Health. 2021; 19(1): 394. doi: 10.3390/ijerph19010394.
Matsugaki R, Fujino Y, Zaitsu M, Saeki S, Matsuda S, Ogami A. Frailty is a risk factor for occupational falls among older workers: an internet-based prospective cohort study. J Occup Health. 2024; 66(1): uiae065. doi: 10.1093/joccuh/uiae065.
Ferrucci L, Walston JD. Frailty. In: Halter JB, Ouslander JG, Studenski S, High KP, Asthana S, Supiano MA, et al, Editors. Hazzard’s geriatric medicine and gerontology. 8th Ed. New York: McGraw-Hill; 2022; Chapter 42.
Nejatinamini S, Campbell DJT, Godley J, Minaker LM, Sajobi TT, McCormack GR, et al. The contribution of modifiable risk factors to socioeconomic inequities in cardiovascular disease morbidity and mortality: a nationally representative population-based cohort study. Prev Med. 2023; 171: 107497. doi:10.1016/j.ypmed.2023.107497
Khadilkar SS. Musculoskeletal disorders and menopause. J Obstet Gynaecol India. 2019; 69(2): 99-103. doi: 10.1007/s13224-019-01213-7.
Greco EA, Pietschmann P, Migliaccio S. Osteoporosis and sarcopenia increase frailty syndrome in the elderly. Front Endocrinol (Lausanne). 2019; 10: 255. doi: 10.3389/fendo.2019.00255.
Blumer J, Le B. Rethinking sarcopenia and frailty of the elderly. Post Reprod Health. 2025; 20533691251337173. doi: 10.1177/20533691251337173.
Singhal S, Singh S, Dewangan GC, Dey S, Banerjee J, Lee J, et al. The prevalence of frailty and its relationship with sociodemographic factors, regional healthcare disparities, and healthcare utilization in the aging population across India. Aging Med (Milton). 2023; 6(3): 212-21. doi:10.1002/agm2.12263.
Eyigor S, Kutsal YG, Duran E, Huner B, Paker N, Durmus B, et al. Frailty prevalence and related factors in the older adult-FrailTURK Project. Age (Dordr). 2015; 37(3): 9791. doi: 10.1007/s11357-015-9791-z.
Lee YS, Chen YM, Chou YY, Lin CS, Chen JP, Kuo FH, et al. Prefrailty subtypes differentially predict 5-year mortality in the functionally independent geriatric population. Arch Gerontol Geriatr. 2023; 106: 104897. doi: 10.1016/j.archger.2022.104897.
Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011; 155(2): 97-107. doi: 10.7326/0003-4819-155-2-201107190-00005.