Psychometric properties of the Thai version of Allen Cognitive Level Screen-5 (Thai ACLS-5) for individuals with schizophrenia
Main Article Content
Abstract
Background: Cognitive impairment is a critical concern for individuals with schizophrenia, affecting their occupational performance, daily activities, and the potential for rehabilitation and skill development. The Allen Cognitive Level Screen-5 (ACLS-5) is a standardized, performance-based assessment designed to evaluate functional cognitive abilities and limitations, providing guidance for individualized interventions. However, there is currently no Thai translation for the ACLS-5.
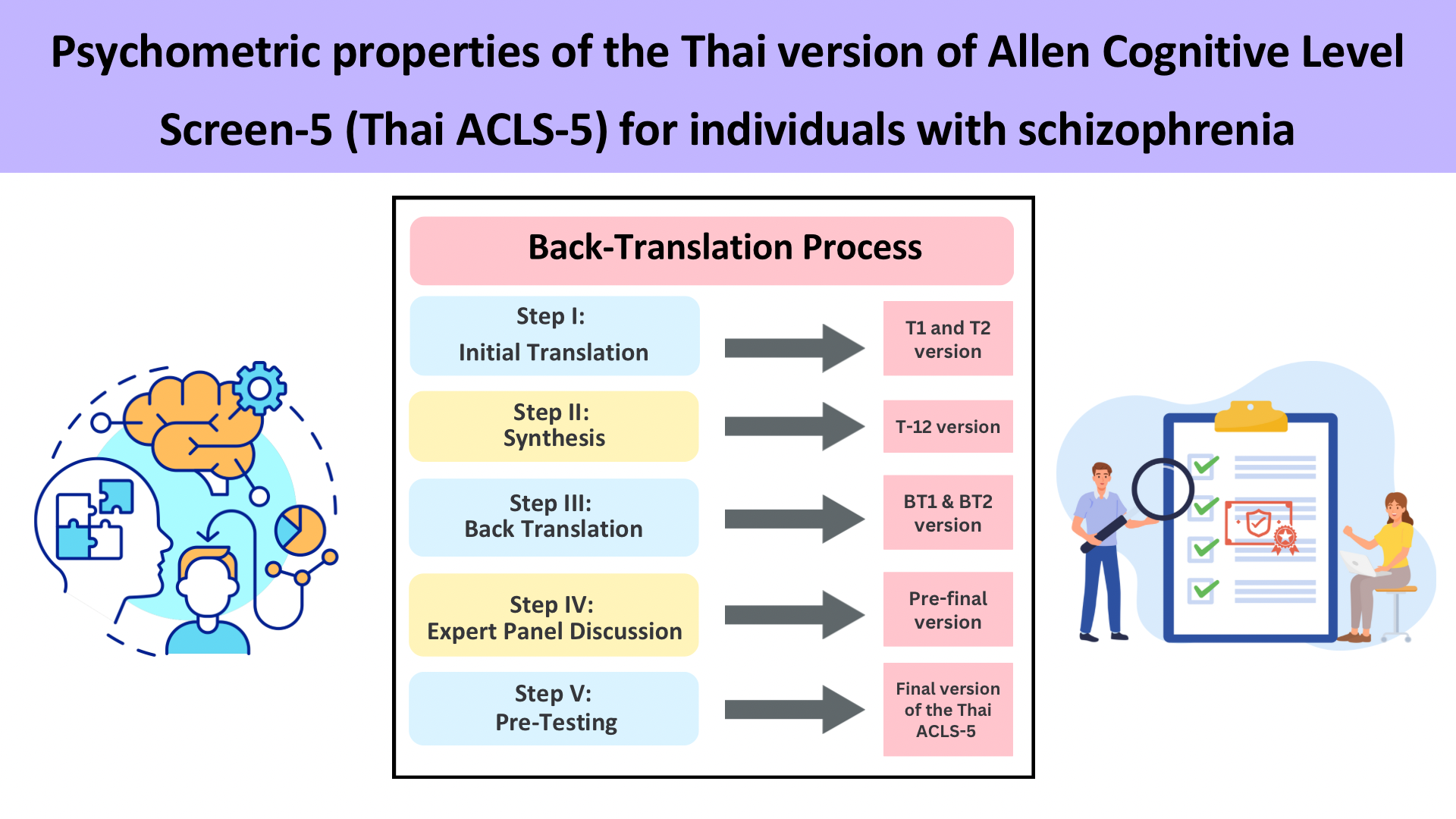
Objectives: This study aimed to translate the ACLS-5 into Thai using a back-translation method and to evaluate its psychometric properties, focusing on construct validity and inter-rater reliability, to ensure its suitability for use in Thai clinical settings.
Materials and methods: The ACLS-5 was translated from English into Thai following Beaton’s protocol, a five-step process for cross-cultural adaptation, and the pre-final version was tested on a sample of 30 individuals with schizophrenia to assess cultural adaptation and content validity. Construct validity was evaluated using a sample of 102 participants, comprising of 51 individuals with schizophrenia and 51 healthy individuals. Inter-rater reliability was examined by two occupational therapists who independently evaluated 38 participants from the schizophrenia group.
Results: In the translation and cultural adaptation phase, the names of the stitching tasks were modified to match Thai culture. Feedback from the Allen Cognitive Group suggested that the terms lacked direct Thai equivalents; consequently, they
remained in their original English form. The pre-final Thai ACLS-5 was tested with 30 individuals with schizophrenia, in which it was reported that the instructions were clear and easy to understand. The Mann-Whitney U test indicated a significant difference in construct validity between individuals with schizophrenia and healthy controls (Z=-6.511, p<0.000), confirming the assessment’s effectiveness in distinguishing cognitive impairment. The intraclass correlation coefficient (ICC) for inter-rater reliability was 0.932, demonstrating excellent reliability.
Conclusion: These findings confirm that the Thai ACLS-5 is a valid and reliable assessment for evaluating functional cognition in individuals with schizophrenia. It allows for a quick and effective assessment of functional cognition in clinical settings. Future research should examine usage in different populations to further establish its utilization.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Medalia A, Revheim N. Dealing with cognitive dysfunction associated with psychiatric disabilities. Walter Boppert: The New York State Office of Mental Health Family; 2002.
Bowie CR, Harvey PD. Cognitive deficits and functional outcome in schizophrenia. Neuropsychiatr Dis Treat. 2006; 2(4): 531-6. doi: 10.2147/nedt.2006.2.4.531.
Shimada T, Ohori M, Inagaki Y, Shimooka Y, Sugimura N, Ishihara I, et al. A multicenter, randomized controlled trial of individualized occupational therapy for patients with schizophrenia in Japan. PLoS One. 2018; 13(10): e0205549. doi: 10.1371/journal.pone.0193869.
Lexen A, Bejerholm U. Occupational engagement and cognitive functioning among persons with schizophrenia: an explorative study. Scand J Occup Ther. 2018; 25(3): 172-9. doi: 10.1080/11038128.2017.1290135.
American Occupational Therapy Association. Role of OT in assessing functional cognition. 2021. Available from: https://www.aota.org/practice/practice-essentials/payment-policy/medicare1/medicare---role-of-ot-in-assessing-functional-cognition.
Pitman T. Mini-Mental State Examination and Large Allen Cognitive Level Screen: predictive validity for discharge disposition among patients of a skilled nursing facility. Tacoma, WA: University of Puget Sound; 2010.
Bakkour N, Samp J, Akhras K, El Hammi E, Soussi I, Zahra F, et al. Systematic review of appropriate cognitive assessment instruments used in clinical trials of schizophrenia, major depressive disorder and bipolar disorder. Psychiatry Res. 2014; 216(3): 291-302. doi: 10.1016/j.psychres.2014.02.014.
Allen CK, Austin SL, David SK, Earhart CA, McCraith DB, Riska-Williams L. Manual for the Allen Cognitive Level Screen-5 (ACLS-5) and Large Allen Cognitive Level Screen-5 (LACLS-5). Camarillo, CA: ACLS and LACLS Committee; 2007.
Rojo-Mota G, Pedrero-Perez EJ, Huertas-Hoyas E, Merritt B, MacKenzie D. Allen Cognitive Level Screen for the classification of subjects treated for addiction. Scand J Occup Ther. 2017; 24(4): 290-8. doi: 10.3109/11038128.2016.1161071.
Scanlan JN, Still M. Functional profile of mental healthconsumers assessed by occupational therapists: level of independence and associations with functional cognition. Psychiatry Res. 2013; 208(1): 29-32. doi: 10.1016/j.psychres.2013.02.032.
Williams LR, Earhart CA, David SK. ACLS-5 and LACLS-5 Test: psychometric properties and use of scores for evidence-based practice 2018. Available from: https://allencognitive.com/wp-content/uploads/CopyrightIVReportfPsychometricsACLS-5_6-12-2016.pdf.
Leung SB, Man DWK. Validity of the Chinese Version of the Allen Cognitive Level Screen Assessment for individuals with schizophrenia. Occup Ther J Res. 2007;27(1): 31-40. doi: 10.1177/153944920702700105.
Chan CL, Ray S, Trudeau S. The development and reliability of the Cantonese version of the Allen Cognitive Level Screen. Occup Ther Int. 2001; 8(4):287-300. doi: 10.1002/oti.152.
Ozturk KL, Bumin G, Ozturk E, Akyurek G. Investigation of the validity and reliability of the Turkish adaptation of Allen Cognitive Level Screen-5 (ACLS-5) with individuals with schizophrenia. Occup Ther Ment Healt. 2022; 39(4): 1-17. doi: 10.1080/0164212X.2022.2135671.
Beaton D, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000; 25(24): 3186-91. doi: 10.1097/00007632-200012150-00014.
Katz N, Toglia J. Cognition, occupation, and participation across the life span: neuroscience, neurorehabilitation, and models of intervention in occupational therapy. 4th ed. North Bethesda, MA: AOTA Press; 2018.
Nilchaikovit T., Uneanong S., Kessawai D., Thomyangkoon P. The Thai version of the Positive and Negative Syndrome Scale (PANSS) for schizophrenia: criterion validity and interrater reliability. J Med Assoc Thai. 2000; 83(6): 646-51. PMID: 10932491.
Kitreerawutiwong N. Public health research: from principle to practice. Phitsanulok: Naresuan University Publishing House; 2017.
Sachs G, Bannick G, Maihofer EIJ, Voracek M, Purdon SE, Erfurth A. Dimensionality analysis of the German version of the Screen for Cognitive Impairment in Psychiatry (SCIP-G) Schizophr Res Cognition. 2022; 29: 1-6. doi: 10.1016/j.scog.2022.100259.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15(2): 155-63. doi: 10.1016/ j.jcm.2016.02.012.
Stewart K, Hancock N, Stancliffe RJ. Factors related to hospital utilisation for people living with schizophrenia: examining Allen’s Cognitive Level Scores, recommended supports and routinely collected variables. Aust Occup Ther J. 2019; 66(5): 591-602. doi: 10.1111/1440-1630.12597.