Correlations between plasma clusterin levels and liver fibrosis in people living with HIV
Main Article Content
Abstract
Background: Chronic liver disease has become a major health concern in people living with human immunodeficiency virus (PLWH). Clusterin has been involved in various pathologic conditions and its contributory role in liver complications in PLWH is still unclear.
Objective: This study aimed to detect plasma clusterin levels and assess their correlation with liver fibrosis in Thai PLWH.
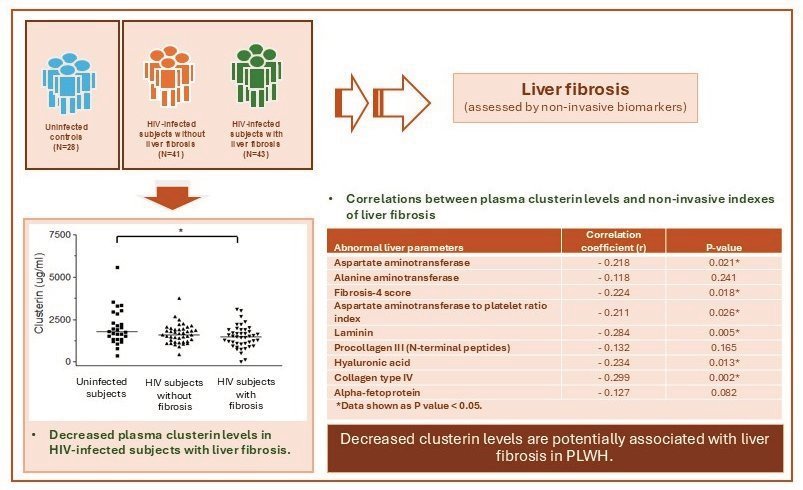
Materials and methods: The study was conducted on 112 subjects, HIV-infected groups with (N=43) and without liver fibrosis (N=41), and uninfected controls (N=28). The subjects were evaluated for liver fibrosis using fibrosis-4 (FIB-4) score and aspartate aminotransferase to platelet ratio index (APRI), together with extracellular matrix fibrosis markers, laminin (LN), procollagen type III N-terminal peptide (PIIINP), hyaluronic acid (HA) and type IV collagen (IVC) and measured for plasma clusterin levels using an enzyme-linked immunosorbent assay.
Results: This study reported that medians of clusterin levels in uninfected controls, and the HIV patient groups without and with liver fibrosis were 1,779.38 (373.07-5,578.69), 1,602.73 (445.28-3,738.33) and 1,487.17 (0-3,111.33) μg/mL, respectively. Kruskal-Wallis test demonstrated a downward trend of clusterin levels in the HIV-infected groups without liver fibrosis and a significantly decreased level in the group with liver fibrosis (p<0.05), compared to those in uninfected controls. Pearson’s correlation analysis indicated negative correlations of clusterin levels with fibrosis markers, FIB-4 score (r=-0.224, p=0.018), APRI (r=-0.211, p=0.026), LN (r=-0.284, P=0.005), HA (r=-0.234, p=0.013) and IVC (r=-0.299, p=0.002).
Conclusion: The study reported the lower levels of plasma clusterin in PLWH who develop liver fibrosis and their correlations with liver fibrosis assessed by the non-invasive markers.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
UNAIDS. Global HIV & AIDS statistics-Fact sheet. 2023. Available from: https://www.unaids.org/en/resources/fact-sheet.
Rodes B, Cadinanos J, Esteban-Cantos A, Rodriguez-Centeno J, Arribas JR. Ageing with HIV: Challenges and biomarkers. EBioMedicine. 2022; 77: 103896 doi: 10.1016/j.ebiom.2022.103896.
Zicari S, Sessa L, Cotugno N, Ruggiero A, Morrocchi E, Concato C, et al. Immune Activation, Inflammation, and Non-AIDS Co-Morbidities in HIV-Infected Patients under Long-Term ART. Viruses. 2019; 11(3): 200. doi: 10.3390/v11030200.
Sherman KE, Thomas DL. HIV and liver disease: a comprehensive update. Top Antivir Med. 2022; 30(4): 547-58. Available from: https://www.ncbi.nlm.nih.gov/pubmed/36375129.
Chamroonkul N, Bansal MB. HIV and the liver. Nat Rev Gastroenterol Hepatol. 2019; 16(1): 1-2. doi: 10.1038/s41575-018-0085-7.
Nallagangula KS, Nagaraj SK, Venkataswamy L, Chandrappa M. Liver fibrosis: a compilation on the biomarkers status and their significance during disease progression. Future science OA. 2018; 4(1): FSO250. doi: 10.4155/fsoa-2017-0083.
Lai JC, Liang LY, Wong GL. Noninvasive tests for liver fibrosis in 2024: are there different scales for different diseases? Gastroenterol Rep (Oxf). 2024; 12:goae024. doi: 10.1093/gastro/goae024.
Ma HY, Dong L, Quan SZ, Li RY, Wang XR. Comparison of four markers of hepatic fibrosis and hepatic function indices in patients with liver cirrhosis and hepatoma. Ann Palliat Med. 2021; 10(4): 4108-21. doi:10.21037/apm-20-1623.
Dong H, Xu C, Zhou W, Liao Y, Cao J, Li Z, et al. The combination of 5 serum markers compared to FibroScan to predict significant liver fibrosis in patients with chronic hepatitis B virus. Clin Chim Acta. 2018; 483: 145-50. doi: 10.1016/j.cca.2018.04.036.
Liao Y, Gong J, Zhou W, Dong H, Liang J, Luo M, et al. Serum liver fibrosis markers discriminate significant liver inflammation in chronic hepatitis B patients with normal or near-normal alanine aminotransferase. J Med Virol. 2019; 91(4): 642-9. doi:10.1002/jmv.25364.
Aigelsreiter A, Janig E, Sostaric J, Pichler M, Unterthor D, Halasz J, et al. Clusterin expression in cholestasis, hepatocellular carcinoma and liver fibrosis. Histopathology. 2009; 54(5): 561-70. doi: 10.1111/j.1365-2559.2009.03258.x.
Materia S, Cater MA, Klomp LW, Mercer JF, La Fontaine S. Clusterin (apolipoprotein J), a molecular chaperone that facilitates degradation of the copper-ATPases ATP7A and ATP7B. J Biol Chem. 2011; 286(12): 10073-83. doi: 10.1074/jbc.M110.190546.
Rohne P, Prochnow H, Koch-Brandt C. The CLU-files: disentanglement of a mystery. Biomol Concepts. 2016; 7(1): 1-15. doi: 10.1515/bmc-2015-0026.
Kang YK, Hong SW, Lee H, Kim WH. Overexpression of clusterin in human hepatocellular carcinoma. Hum Pathol. 2004 ; 35(11): 1340-6. doi: 10.1016/j.humpath.2004.07.021.
Satapathy S, Wilson MR. The Dual Roles of Clusterin in Extracellular and Intracellular Proteostasis. Trends Biochem Sci. 2021; 46(8) :652-60. doi: 10.1016/j.tibs.2021.01.005.
Redondo M, Villar E, Torres-Munoz J, Tellez T, Morell M, Petito CK. Overexpression of clusterin in human breast carcinoma. Am J Pathol. 2000; 157(2): 393-9. doi: 10.1016/S0002-9440(10)64552-X.
Kropackova T, Mann H, Ruzickova O, Sleglova O, Vernerova L, Horvathova V, et al. Clusterin serum levels are elevated in patients with early rheumatoid arthritis and predict disease activity and treatment response. Sci Rep. 2021; 11(1): 11525. doi: 10.1038/s41598-021-90973-2.
Liu H, Li Y, Gao F, Meng P, Yu H, Wu T, et al. Serum Clusterin: A Potential Marker for Assessing the Clinical Severity and Short-Term Prognosis of Hepatitis B Virus-Related Acute-on-Chronic Liver Failure. Dis Markers. 2020; 2020: 8814841. doi: 10.1155/2020/8814841.
So A, Sinnemann S, Huntsman D, Fazli L, Gleave M. Knockdown of the cytoprotective chaperone, clusterin, chemosensitizes human breast cancer cells both in vitro and in vivo. Mol Cancer Ther. 2005; 4(12): 1837-49. doi: 10.1158/1535-7163.MCT-05-0178.
Mlambo ZP, Varaden D, Moodley J, Naicker T. Are concentrations of clusterin and beta-2-glycoprotein I dysregulated in HIV associated preeclampsia? Eur J Obstet Gynecol Reprod Biol. 2020; 251: 1-7. doi: 10.1016/j.ejogrb.2020.03.036.
Torres-Munoz JE, Redondo M, Czeisler C, Roberts B, Tacoronte N, Petito CK. Upregulation of glial clusterin in brains of patients with AIDs. Brain Res. 2001; 888(2): 297-301. doi:10.1016/s0006-8993(00)03052-3.
Foca E, Fabbiani M, Prosperi M, Quiros Roldan E, Castelli F, Maggiolo F, et al. Liver fibrosis progression and clinical outcomes are intertwined: role of CD4+ T-cell count and NRTI exposure from a large cohort of HIV/HCV-coinfected patients with detectable HCV-RNA: A MASTER cohort study. Medicine (Baltimore). 2016; 95(29): e4091. doi: 10.1097/MD.0000000000004091.
Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006; 43(6): 1317-25. doi: 10.1002/hep.21178.
Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003; 38(2): 518-26. doi: 10.1053/jhep.2003.50346.
Akekawatchai C, Changsri K, Tunkor A, Phuegsilp C, Soimanee T, Fungkraja M, et al. Lack of Association between IFN-gamma, CXCL10 and TGF-beta1 Gene Polymorphisms and Liver Complication in HIV-infected Thais. Asian Pac J Cancer Prev. 2022; 23(4): 1279-84. doi: 10.31557/APJCP.2022.23.4.1279.
Akekawatchai C, Sretapunya W, Pipatsatitpong D, Chuenchit T. Hepatitis B or C virus coinfection in and risks for transaminitis in human immunodeficiency virus - infected Thais on combined antiretroviral therapy. Asian Biomedicine. 2015; 9(3): 353-61.
Chiraunyanann T, Changsri K, Sretapunya W, Yuen-yongchaiwat K, Akekawatchai C. CXCL12 G801A polymorphism is associated with significant liver fibrosis in HIV-infected Thais: a cross-sectional study. Asian Pac J Allergy Immunol. 2019; 37(3): 162-70. doi: 10.12932/AP-160917-0162.
Roehlen N, Crouchet E, Baumert TF. Liver Fibrosis: Mechanistic Concepts and Therapeutic Perspectives. Cells. 2020; 9(4): 875. doi:10.3390/cells9040875.
Gruevska A, Moragrega AB, Cossarizza A, Esplugues JV, Blas-Garcia A, Apostolova N. Apoptosis of Hepatocytes: Relevance for HIV-Infected Patients under Treatment. Cells. 2021; 10(2): 410. doi: 10.3390/cells10020410.
Cunin P, Beauvillain C, Miot C, Augusto JF, Preisser L, Blanchard S, et al. Clusterin facilitates apoptotic cell clearance and prevents apoptotic cell-induced autoimmune responses. Cell death & disease. 2016; 7(5): e2215. doi: 10.1038/cddis.2016.113.
Sintich SM, Steinberg J, Kozlowski JM, Lee C, Pruden S, Sayeed S, et al. Cytotoxic sensitivity to tumor necrosis factor-alpha in PC3 and LNCaP prostatic cancer cells is regulated by extracellular levels of SGP-2 (clusterin). Prostate. 1999; 39(2): 87-93. doi:10.1002/(sici)1097-0045(19990501)39:2<87::aid-pros2>3.0.co;2-z.
Burkey BF, Stuart WD, Harmony JA. Hepatic apolipoprotein J is secreted as a lipoprotein. J Lipid Res. 1992; 33(10): 1517-26. Available from: https://www.ncbi.nlm.nih.gov/pubmed/1431576.
Fernandez Encinas L, Lluch N, Wu AHB, Kaski JC, Badimon L, Cubedo J. A Novel ELISA for the Quantification of Serum Levels of 2 Glycosylated Variants of Apolipoprotein J: Biomarkers for Myocardial Ischemia. J Appl Lab Med. 2023; 8(5): 917-30. doi: 10.1093/jalm/jfad034.