Efficacy of rehabilitation in improving social cognition and behavioral outcomes of pediatric traumatic brain injury: An integrative review
Main Article Content
Abstract
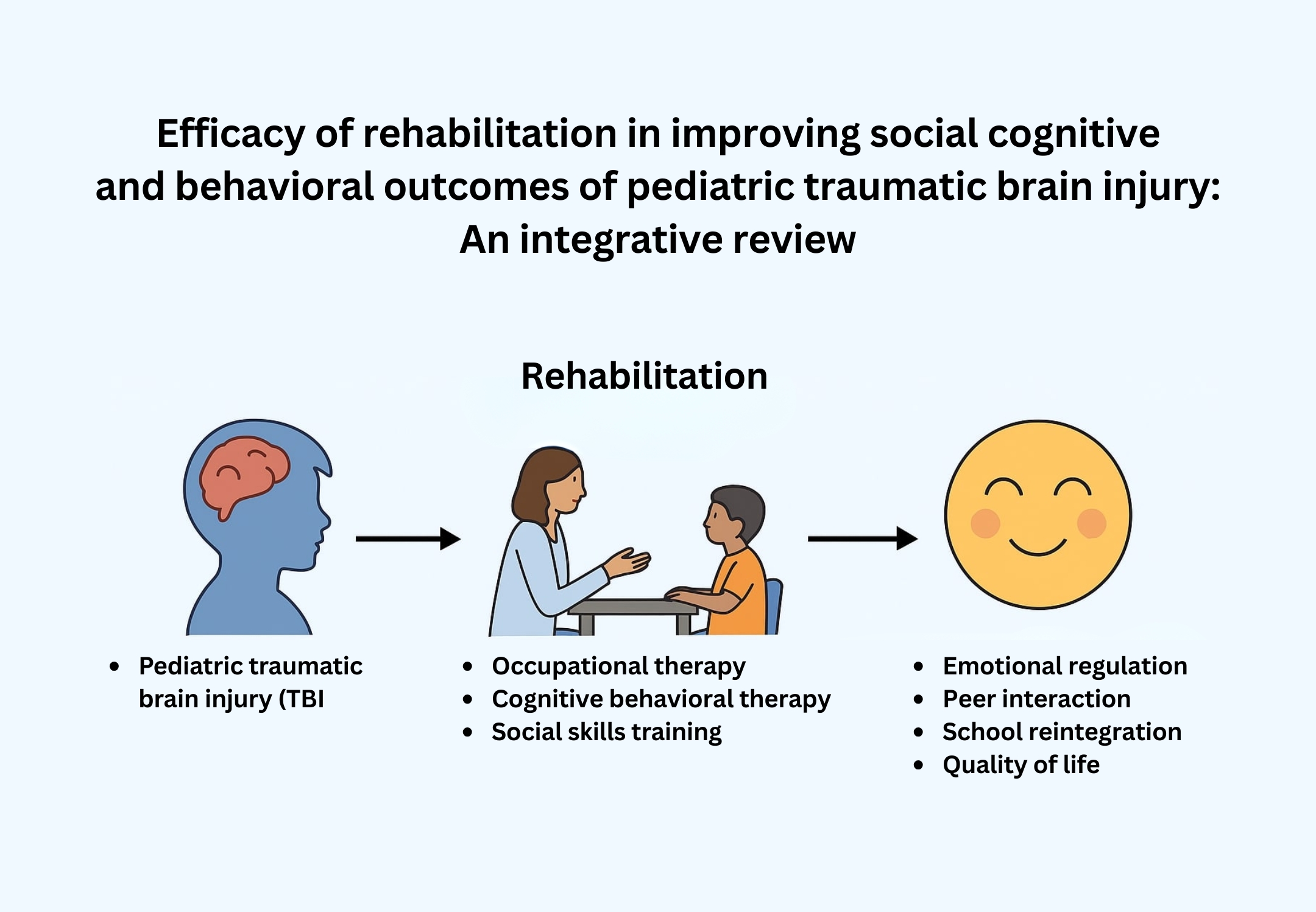
Background: One of the main causes of long-term disability in kids and teenagers is pediatric traumatic brain injury (TBI), which frequently leads to deficiencies in behavioural and social cognition. Rehabilitation helps in enhancing these outcomes.
Objectives: The purpose of this integrative review is to assess the available data on how well rehabilitation works to improve behavioral and social cognition in children with traumatic brain injury.
Materials and methods: An extensive search of electronic databases and registries (PubMed, Scopus, Google Scholar, and Web of Science, among others) was conducted. Studies that looked at how rehabilitation therapies affected the social cognition and behavioural outcomes of pediatric TBI published between 2010 and 2024 were included.
Results: Eighteen studies met the inclusion criteria, which encompassed various rehabilitation interventions, including family-based interventions, social skills training, neurocognitive remediation, and cognitive-behavioural therapy (CBT). Overall, both behavioural outcomes, such as emotional regulation and adaptive behaviours, as well as social cognition, including theory of mind, emotional recognition, and social problem-solving abilities, were shown to improve with rehabilitation.
Conclusion: In children and adolescents with TBI, rehabilitation interventions-especially those centered on social skills training, cognitive-behavioural methods, and neurocognitive remediation-can greatly enhance social cognition and behavioural outcomes. The analysis underscores the necessity of customized, multidisciplinary rehabilitation programs and identifies research topics for the future, such as including neurobiological underpinnings and long-term monitoring to gauge how long therapy effects last.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Gardner MT, O’Meara AM, Miller Ferguson N. Pediatric traumatic brain injury: an update on management. Curr Pediatr Rep. 2017; 5(4): 213-9. doi: 10.1007/s40124-017-0144-5.
Anderson V, Moore C. Age at injury as a predictor of outcome following pediatric head injury: a longitudinal perspective. Child Neuropsychol. 1995; 1(3): 187-202. doi: 10.1080/09297049508400224.
Li L, Liu J. The effect of pediatric traumatic brain injury on behavioural outcomes: a systematic review. Dev Med Child Neurol. 2013; 55(1): 37-45. doi: 10.1111/j.1469-8749.2012.04414.x.
Langlois JA, Rutland-Brown W, Thomas KE. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2006. Available from: https://stacks.cdc.gov/view/cdc/12294
Bechtel K, Stoessel K, Leventhal JM, et al. Characteristics that distinguish accidental from abusive injury in hospitalized young children with head trauma. Pediatrics. 2004; 114(1): 165-8. doi: 10.1542/peds.114.1.165.
Billmire ME, Myers PA. Serious head injury in infants–accident or abuse? Pediatrics. 1985; 75(2): 340-2. doi: 10.1007/BF00335074 .
Laatsch L, Harrington D, Hotz G, Marcantuono J, Mozzoni MP, Walsh V, et al. An evidence-based review of cognitive and behavioural rehabilitation treatment studies in children with acquired brain injury. J Head Trauma Rehabil. 2007; 22(4): 248-56. doi: 10.1097/01.HTR.0000281841.92720.0a.
Fuentes MM, Wang J, Haarbauer-Krupa J, Yeates KO, Durbin D, Zonfrillo MR, et al. Unmet rehabilitation needs after hospitalization for traumatic brain injury. Pediatrics. 2018; 141(5): e20172859. doi: 10.1542/peds.2017-2859.
Laatsch L, Dodd J, Brown T, Ciccia A, Connor F, Davis K, et al. Evidence-based systematic review of cognitive rehabilitation, emotional, and family treatment studies for children with acquired brain injury literature: From 2006 to 2017. Neuropsychol Rehabil. 2020; 30(1): 130-61. doi: 10.1080/09602011.2019.1678490.
DeLisa JA, Gans BM, Walsh NE. Physical medicine and rehabilitation: principles and practice. 4th Ed. Philadelphia: Lippincott Williams & Wilkins; 2005.
Köhler R, Wilhelm EE, Shoulson I. Cognitive Rehabilitation Therapy for Traumatic Brain Injury: Evaluating the Evidence. Washington, DC: National Academies Press; 2012. doi: 10.17226/13220.
Schretlen DJ, Shapiro AM. A quantitative review of the effects of traumatic brain injury on cognitive functioning. Int Rev Psychiatry. 2003; 15(4): 341-9. doi: 10.1080/09540260310001606728.
Vaishnavi S, Rao V, Fann JR. Neuropsychiatric problems after traumatic brain injury: unraveling the silent epidemic. Psychosomatics. 2009; 50(3): 198-205. doi: 10.1176/appi.psy.50.3.198.
Barman A, Chatterjee A, Bhide R. Cognitive impairment and rehabilitation strategies after traumatic brain injury. Indian J Psychol Med. 2016; 38(3): 172-81. doi: 10.4103/0253-7176.183086.
Chan DY, Fong KN. The effects of problem-solving skills training based on metacognitive principles for children with acquired brain injury attending mainstream schools: a controlled clinical trial. Disability and Rehabilitation. 2011; 33(21-22): 2023-32. doi: 10.3109/09638288.2011.556207.
Hanten G, Bartha M, Levin HS. Metacognition following pediatric traumatic brain injury: a preliminary study. Dev Neuropsychol. 2000;18(3):383–98. doi: 10.1207/S1532694206Hanten
Popernack ML, Gray N, Reuter-Rice K. Moderate-to-severe traumatic brain injury in children: complications and rehabilitation strategies. J Pediatr Health Care. 2015; 29(3): e1-7. doi: 10.1016/j.pedhc.2014.09.003.
Resch C, Rosema S, Hurks P, de Kloet A, van Heugten C. Searching for effective components of cognitive rehabilitation for children and adolescents with acquired brain injury: a systematic review. Brain Inj. 2018; 32(6): 679-92. doi: 10.1080/02699052.2018.1458335.
Wang C, Li X, Liu Y. Influence of play-based metaphors on negative emotion and behaviour in children recovering from brain injury. Chinese J Child Health Care. 2024; 32(5): 566-71. doi: 10.11852/zgetbjzz2023-0742.
Sood NT, Godfrey C, Krasts D, Morrison E, Chavez Arana C, Hearps SJ, et al. Rehabilitation of Executive Function in Pediatric Traumatic Brain Injury (REPeaT): outcomes of a pilot randomized controlled trial. Neuropsychology. 2024; 38(5): 392-402. doi: 10.1037/neu0000951.
Sargénius HL, Andersson S, Haugen I, Hypher R, Brandt AE, Finnanger TG, et al. Cognitive rehabilitation in paediatric acquired brain injury-a 2-year follow-up of a randomized controlled trial. Front Neurol. 2023;14: 1173480. doi: 10.3389/fneur.2023.1173480.
On ZX, Ryan NP, Konjarski M, Catroppa C, Stargatt R. Social cognition in paediatric traumatic brain injury: A systematic review and meta-analysis. Neuropsychol Rev. 2022;32(4):924-945. doi:10.1007/s11065-022-09553-1
Polinder S, Cnossen MC, Real RGL, Covic A, Gorbunova A, Voormolen D, et al. A multidimensional approach to post-concussion symptoms in mild traumatic brain injury. Front Neurol. 2018; 9: 1113. doi: 10.3389/fneur.2018.01113.
Séguin M, Lahaie A, Matte-Gagné C, Beauchamp MH. Ready! Set? Let’s Train!: Feasibility of an intensive attention training program and its beneficial effect after childhood traumatic brain injury. Ann Phys Rehabil Med. 2018; 61(4): 189-96. doi: 10.1016/j.rehab.2017.05.001.
Ryan NP, van Bijnen L, Catroppa C, Beauchamp MH, Crossley L, Hearps SJ, et al. Longitudinal outcome and recovery of social problems after pediatric traumatic brain injury (TBI): Contribution of brain insult and family environment. Int J Dev Neurosci. 2016; 49: 23-30. doi: 10.1016/j.ijdevneu.2015.12.004.
Brown FL, Whittingham K, Boyd RN, McKinlay L, Sofronoff K. Does Stepping Stones Triple P plus Acceptance and Commitment Therapy improve parent, couple, and family adjustment following paediatric acquired brain injury? A randomised controlled trial. Behav Res Ther. 2015; 73: 58-66. doi: 10.1016/j.brat.2015.07.001.
Coyne JH, Borg JM, DeLuca J, Glass L, Sumowski JF. Retrieval practice as an effective memory strategy in children and adolescents with traumatic brain injury. Arch Phys Med Rehabil. 2015; 96(4): 742-5. doi: 10.1016/j.apmr.2014.09.022.
Cook LG, Chapman SB, Elliott AC, Evenson NN, Vinton K. Cognitive gains from gist reasoning training in adolescents with chronic-stage traumatic brain injury. Front Neurol. 2014; 5: 87. doi: 10.3389/fneur.2014.00087.
Krasny-Pacini A, Limond J, Evans J, Hiebel J, Bendjelida K, Chevignard M. Context-sensitive goal management training for everyday executive dysfunction in children after severe traumatic brain injury. J Head Trauma Rehabil. 2014; 29(5): E49-64. doi: 10.1097/HTR.0000000000000015.
Bower J, Catroppa C, Grocke D, Shoemark H. Music therapy for early cognitive rehabilitation post-childhood TBI: an intrinsic mixed methods case study. Dev Neurorehabil. 2014; 17(5): 339-46. doi: 10.3109/17518423.2013.778910.
Haslam C, Bazen-Peters C, Wright I. Errorless learning improves memory performance in children with acquired brain injury: a controlled comparison of standard and self-generation techniques. Neuropsychol Rehabil. 2012; 22(5): 697-715. doi: 10.1080/09602011.2012.686820.
Ho J, Epps A, Parry L, Poole M, Lah S. Rehabilitation of everyday memory deficits in paediatric brain injury: self-instruction and diary training. Neuropsychol Rehabil. 2011; 21(2): 183-207. doi: 10.1080/09602011.2010.547345.
Feeney TJ. Structured flexibility: the use of context-sensitive self-regulatory scripts to support young persons with acquired brain injury and behavioural difficulties. J Head Trauma Rehabil. 2010; 25(6): 416-25. doi: 10.1097/HTR.0b013e3181fbc0a2.
Yeates KO, Taylor HG, Walz NC, Stancin T, Wade SL. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010; 24(3): 345-56. doi: 10.1037/a0018387.