The effect of exergaming on balance among children with intellectual disability
Main Article Content
Abstract
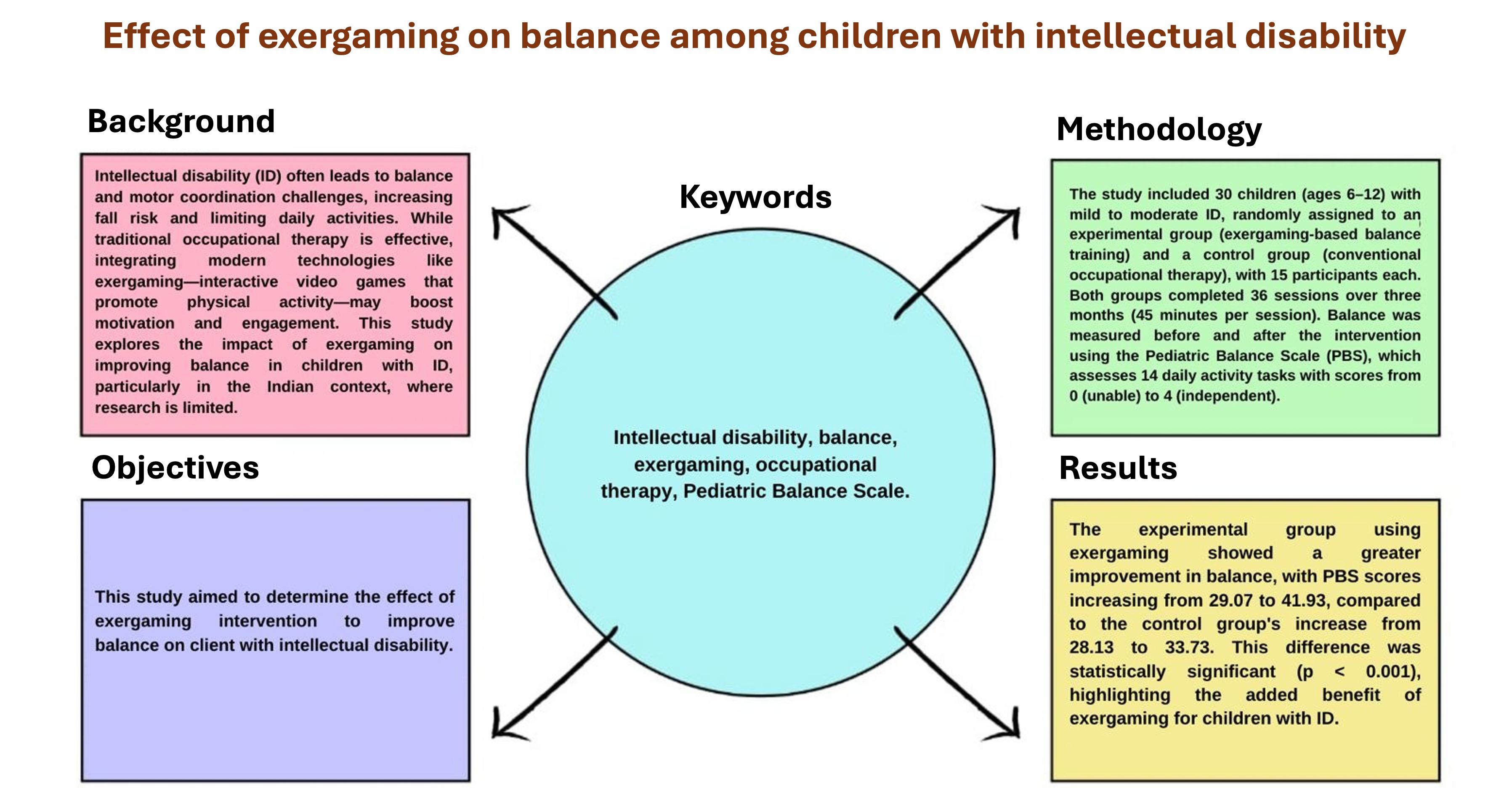
Background: Intellectual disability (ID) is associated with balance and motor coordination challenges, leading to increased fall risk and limitations in daily activities. Traditional occupational therapy interventions have shown efficacy in addressing these issues, but there is a growing interest in integrating modern technologies, such as exergaming, into therapeutic programs. Exergaming combines physical activity with interactive video games, potentially enhancing motivation and engagement among children with ID. This study focuses on
assessing the impact of exergaming on improving balance in children with ID, an area that remains underexplored in the Indian context.
Objectives: This study aimed to determine the effect of an exergaming intervention on improving balance in clients with intellectual disabilities. Materials and methods: The study involved 30 children aged 6-12 years diagnosed with mild to moderate ID. Participants were randomly divided into two groups: the experimental group (N=15) received exergaming-based balance training, and the control group (N=15) underwent conventional occupational therapy. Both groups participated in 36 sessions over three months, each lasting 45 minutes. Balance was assessed using the Pediatric Balance Scale (PBS) before and after the intervention. The PBS includes 14 tasks that evaluate balance through various daily activities, with scores ranging from 0 (unable to perform) to 4 (independent).
Results: The results demonstrated a significant improvement in balance for both groups. However, the experimental group, which engaged in exergaming, showed a more substantial improvement in PBS scores, increasing from a mean of 29.07 to 41.93. In contrast, the control group’s mean PBS score increased from 28.13 to 33.73. Statistical analysis confirmed that the improvement in the experimental group was significantly more significant (p<0.001), indicating the added benefit of exergaming in enhancing balance among children with ID.
Conclusion: The results indicate that exergaming is an effective intervention for improving balance in children with intellectual disabilities, as it offers engaging, challenging, and play-based therapy. Enhancing balance and postural control may also lead to broader physical and cognitive benefits, such as improved cardiovascular health, muscular strength, and cognitive processing.
These improvements can further support functional independence, promoting inclusivity and better community engagement. Ultimately, this study highlights the potential of exergaming to empower individuals with intellectual disabilities, fostering their overall well-being and quality of life.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Johnson KR, Blaskowitz M, Mahoney WJ. Occupational therapy practice with adults with intellectual disability: What more can we do? Open J Occup Ther. 2019; 7: 1-15. doi: 10.15453/2168-6408.1573.
Russell PSS, Nagaraj S, Vengadavaradan A, Russell S, Mammen PM, Shankar SR, et al. Prevalence of intellectual disability in India: A meta-analysis. World J Clin Pediatr. 2022; 11: 206-14. doi: 10.5409/wjcp.v11.i2.206.
Dehghani M, Gunay M. The effect of balance training on static and dynamic balance in children with intellectual disability. J Appl Environ Biol Sci. 2015; 5: 127-31. doi: 10.5958/2249-7315.2015.00108.2
Blomqvist S, Olsson J, Wallin L, Wester A, Rehn B. Adolescents with intellectual disability have reduced postural balance and muscle performance in trunk and lower limbs compared to peers without intellectual disability. Res Dev Disabil. 2013; 34: 198-206. doi: 10.1016/j.ridd.2012.07.008.
Rine RM, Dannenbaum E, Szabo J. 2015 section on pediatrics knowledge translation lecture: Pediatric vestibular-related impairments. Pediatr Phys Ther. 2016; 28: 2-6. doi: 10.1097/PEP.0000000000000226.
Boonyong S, Siu K-C, van Donkelaar P, Chou L-S, Woollacott MH. Development of postural control during gait in typically developing children: the effects of dual-task conditions. Gait Posture. 2012; 35: 428-34. doi: 10.1016/j.gaitpost.2011.11.002.
Karachi C, Grabli D, Bernard FA, Tandé D, Wattiez N, Belaid H, et al. Cholinergic mesencephalic neurons are involved in gait and postural disorders in Parkinson disease. J Clin Invest. 2010; 120: 2745-54. doi: 10. 1172/JCI42642.
Zur O, Ronen A, Melzer I, Carmeli E. Vestibulo-ocular response and balance control in children and young adults with mild-to-moderate intellectual and developmental disability: a pilot study. Res Dev Disabil. 2013; 34: 1951-7. doi: 10.1016/j.ridd.2013.03.007.
Dellavia C, Pallavera A, Orlando F, Sforza C. Postural stability of athletes in special olympics. Percept Mot Skills. 2009; 108: 608-22. doi: 10.2466/PMS.108.2.608-622.
Chiba Y, Shimada A, Yoshida F, Keino H, Hasegawa M, Ikari H, et al. Risk of fall for individuals with intellectual disability. Am J Intellect Dev Disabil. 2009; 114: 225-36. doi: 10.1352/1944-7558-114.4:225-236.
Wajda DA, Motl RW, Sosnoff JJ. Dual task cost of walking is related to fall risk in persons with multiple sclerosis. J Neurol Sci. 2013; 335: 160-3. doi: 10.1016/ j.jns.2013.09.021.
Almuhtaseb S, Oppewal A, Hilgenkamp TIM. Gait characteristics in individuals with intellectual disabilities: a literature review. Res Dev Disabil. 2014; 35: 2858-83. doi: 10.1016/j.ridd.2014.07.017.
Joseph C, Leavy B, Franzén E. Predictors of improved balance performance in persons with Parkinson’s disease following a training intervention: analysis of data from an effectiveness-implementation trial. Clin Rehabil. 2020; 34: 837-44. doi: 10.1177/0269215520917199.
Oppewal A, Hilgenkamp TIM. The association between gait and physical fitness in adults with intellectual disabilities: Gait and physical fitness in adults with intellectual disabilities. J Intellect Disabil Res. 2018; 62: 454-66. doi: 10.1111/jir.12484.
Blomqvist S, Wester A, Rehn B. Postural muscle responses and adaptations to backward platform perturbations in young people with and without intellectual disability. Gait Posture. 2014; 39: 904-8. doi: 10.1016/j.gaitpost. 2013.11.018.
Bogost I. The rhetoric of exergaming. In: DAC’05: Proceedings of the Digital Arts and Cultures Conference; 2005 Dec 1–3; Copenhagen, Denmark. p.51. https://share.google/PggimpB9BECJOQTlL
Hilton CL, Cumpata K, Klohr C, Gaetke S, Artner A, Johnson H, et al. Effects of exergaming on executive function and motor skills in children with autism spectrum disorder: a pilot study. Am J Occup Ther. 2014; 68: 57-65. doi: 10.5014/ajot.2014.008664.
Gao Z, Pope Z, Lee JE, Stodden D, Roncesvalles N, Pasco D, et al. Impact of exergaming on young children’s school day energy expenditure and moderate-to-vigorous physical activity levels. J Sport Health Sci. 2017; 6: 11-6. doi: 10.1016/j.jshs.2016.11.008.
Gao Z, Hannon JC, Newton M, Huang C. Effects of curricular activity on students’ situational motivation and physical activity levels. Res Q Exerc Sport. 2011; 82: 536-44. doi: 10.1080/02701367.2011.10599786.
Gao Z, Chen S, Pasco D, Pope Z. Effects of active video games on physiological and psychological outcomes among children and adolescents: A meta-analysis. Obes Rev. 2015; 16: 783-94.doi:10.1111/obr.12287
Franjoine MR, Gunther JS, Taylor MJ. Pediatric balance scale: a modified version of the berg balance scale for the school-age child with mild to moderate motor impairment. Pediatr Phys Ther. 2003; 15: 114-28. doi: 10.1097/01.PEP.0000068117.48023.18.
Ac Duarte N, Grecco LA, Franco RC, Zanon N, Oliveira CS. Correlation between Pediatric Balance Scale and functional test in children with cerebral palsy. J Phys Ther Sci. 2014; 26: 849-53. doi: 10.1589/jpts.26.849
Benzing V, Schmidt M. Exergaming for children and adolescents: Strengths, weaknesses, opportunities and threats. J Clin Med. 2018; 7: 422. doi: 10.3390/jcm7110422.
Lourenço C, Esteves D, Corredeira R, Seabra A. The effect of a trampoline-based training program on the muscle strength of the inferior limbs and motor proficiency in children with autism spectrum disorders. J Phys Educ Sport. 2015; 15(3): 479-86 doi: 10.7752/jpes.2015.03073.
Vernadakis N, Papastergiou M, Zetou E, Antoniou P. The impact of an exergame-based intervention on children’s fundamental motor skills. Comput Educ. 2015; 83: 90-102. doi: 10.1016/j.compedu.2015.01. 001.
Ferguson MB, Anderson-Hanley PC, Mazurek MO, Parsons S, Warren Z. Game interventions for autism spectrum disorder. Games Health. 2012; 1: 248-53. doi: 10.1089/g4h.2012.0717.
Benzing V, Schmidt M. The effect of exergaming on executive functions in children with ADHD: A randomized clinical trial. Scand J Med Sci Sports. 2019; 29: 1243-53. doi: 10.1111/sms.13446.