Development and validation of a self-assessment instrument for sodium intake in the population aged 30-44 years in 4th Regional Health, Thailand
Main Article Content
Abstract
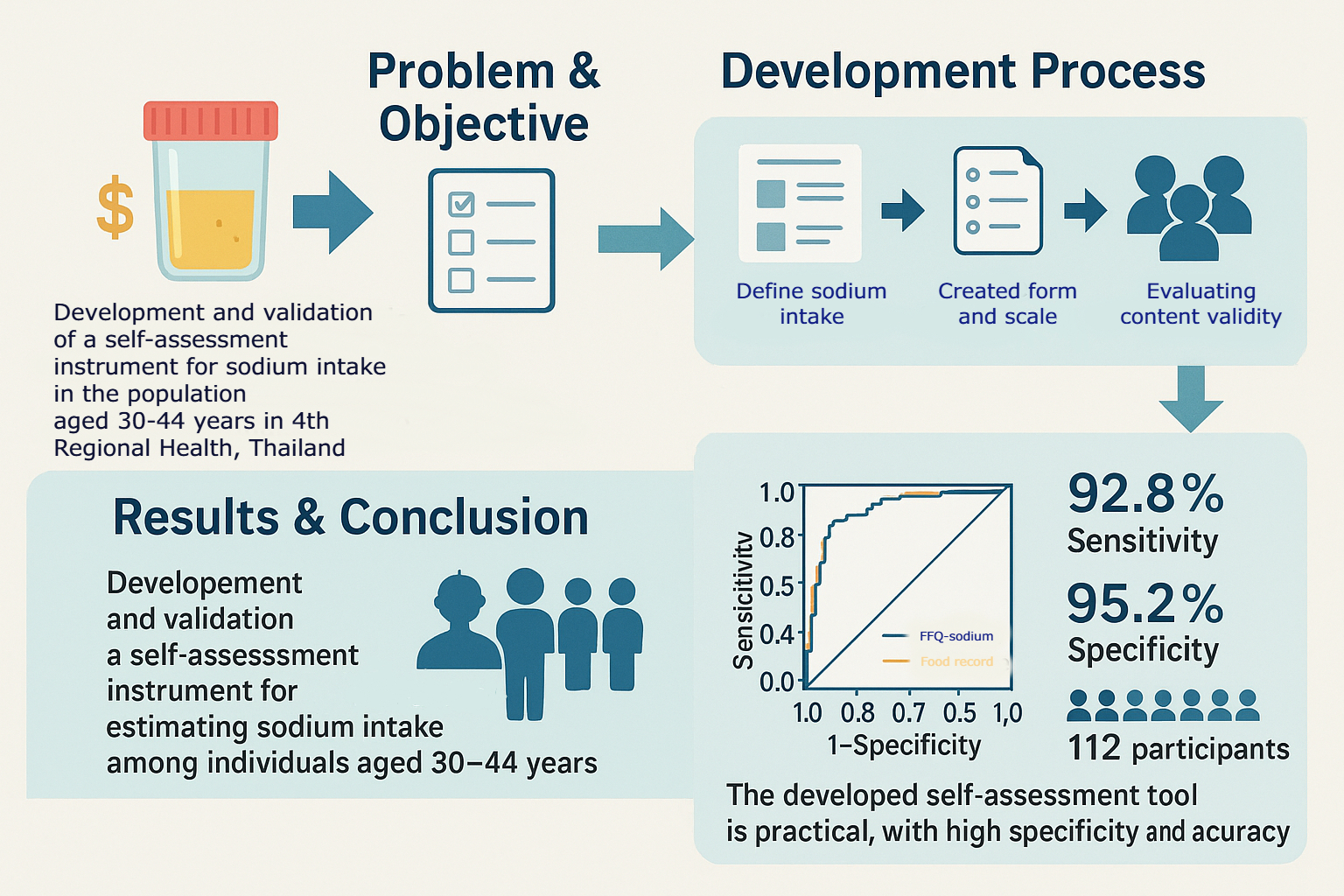
Background: Laboratory-based urine tests are the current standard for assessing sodium intake but are complex and costly. This study aimed to develop a valid, self-assessment questionnaire aligned with laboratory findings using a six-step instrument development process.
Objective: To develop and validate a self-assessment instrument for estimating sodium intake among individuals aged 30–44 years.
Materials and methods: The six-step process involved (1) defining sodium intake by reviewing existing research; (2) creating a list of items based on different food types and how they are eaten; (3) deciding on the format and scale for assessment; (4) checking face validity with feedback from expert advisors; (5) evaluating content validity with five experts and calculating the Item-Objective Congruence (IOC); and (6) testing construct and concurrent validity using ROC analysis.
Results: We categorized a total of 157 food items for inclusion. The questionnaire used a checklist format with frequency ratings (1–7 times/day). Content validity yielded IOC values between 0.6 and 1.0, with 151 items retained. Construct validity showed strong alignment with sodium excretion levels, with a cut-off point of 3.46 and an ROC of 93.3%. Of 120 participants, 112 were correctly classified, yielding 92.8% sensitivity, 95.2% specificity, a 6.7% false positive rate, and 86.7% accuracy (95% CI = 0.880-0.987).
Conclusion: The developed self-assessment tool is practical for single-day dietary evaluation and demonstrates high specificity and accuracy. It offers a reliable, cost-effective alternative for assessing sodium intake at the population level.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Podapon J. Online learning management: The way of education. Mahamakut Royal University; 2020.
Gurdil H, Anadol HO, Soguksu YB. The use of artificial intelligence tools in assessing content validity:
a comparative study with human experts. arXiv [Preprint]. 2025 Feb 3. Available from: https://arxiv. org/abs/2503.15525
Ray P, Le Manach Y, Riou B, Houle TT, Warner DS. Statistical evaluation of a biomarker. Anesthesiology.
;112(4):1023– 40doi: 10.1097ALN.0b013e3181d47604
Jaafar MK, Rahman AR, Nordin N. Correlation between spot urine sodium, 24-hour urinary sodium, and food frequency questionnaire in estimation of salt intake in young healthy individuals. J Hypertens. 2018;36:e288. doi: 10.1097/01.hjh.0000539177.80515.5c
Ministry of Public Health (MOPH). Non-communicable diseases (NCDs) situation in Thailand 2019. [cited 2024 Nov 13]. Available from: http://www.thaincd.com/
World Health Organization. Clinical guidelines for the management of hypertension. Geneva: World Health
Organization; 2005 [cited 2021 Feb 19]. Available from: https://www.who.int/iris/handle/10665/119738
Shahar S, Shahril MR, Abdullah N, Borhanuddin B, Kamaruddin MA, Yusuf NAM, et al. Development and relative validity of a semiquantitative food frequencyquestionnaire to estimate dietary intake among a multi-ethnic population in the Malaysian Cohort Project. Nutrients. 2021;13(4):1163. doi: 10.3390/nu13041163.
Beresford SA, Thompson B, Feng Z, Christianson A, McLerran D, Patrick DL. Development of an assessment tool to measure healthy eating in Navajo children and their families. J Acad Nutr Diet. 2023;123(3):456–65. doi: 10.1016/j.jand.2022.12.005.
McCarron DA, Kazaks AG, Geerling JC, Stern JS, Graudal NA, Dawson-Hughes B. Normal range of human dietary sodium intake: a perspective based on 24-hour urinary sodium excretion worldwide. Am J Hypertens. 2013;26(10):1218–23. doi: 10.1093/ajh/hpt139
McLean RM, Farmer VL, Nettleton A, Cameron CM, Cook NR, Campbell NRC, TRUE Consortium. Assessment
of dietary sodium intake using a food frequency questionnaire and 24-hour urinary sodium excretion: a systematic literature review. J Clin Hypertens. 2017;19(12):1214–30. doi: 10.1111/jch.13136
World Health Organization. WHO Thailand: improving hypertension care cascade with more than 60% control rate through innovation [Internet]. Geneva: World Health Organization; 2023 [cited 2023 Apr 25]. Available from: https://www.who.int/thailand/news/detail/2023/04/25/who-thailand-improvinghypertension-
care-cascade-with-more-than-60-percent-control-rate-through-innovation
Chailimpamontree W, Kantachuvesiri S, Aekplakorn W, et al. Estimated dietary sodium intake in Thailand:
a nationwide population survey with 24-hour urine collections. J Clin Hypertens (Greenwich). 2021;23(4):744–
doi: 10.1111/jch.14147
Nephrology Society of Thailand. Nephrology Meeting 2020. [Conference]. 2020 Nov 13–14. Available from: https://www.nephrothai.org/
Saengyo S, Rerkkasem K, Wungrath J. Effectiveness of a Line application together with telephone-based
consultation and education program on the dietary knowledge and behavior among caregivers of end-stage
renal disease patients on hemodialysis. Malays J Public HealthMed. 2023;23(2):282–90. doi: 10.37268mjphm/
vol.23/no.2/art.1300
Matsuno T, Takachi R, Ishihara J, Ishii Y, Kito K, Maruya S, et al. Validity of the food frequency questionnaire-estimated intakes of sodium, potassium, and sodium-topotassium ratio for screening at a point of absolute intake among middle-aged and older Japanese adults. Nutrients. 2022;14(13):2594. doi: 10.3390/nu14132594
World Health Organization. Global database on body mass index [Internet]. Geneva: World Health Organization; 2021 [cited 2021 Feb 8]. Available from: http://apps. who.int/bmi/index.jsp?introPage=intro_3.html
Huang Y, et al. Measurement error corrected sodium and potassium intake estimation using 24-hour urinary excretion. Hypertension. 2014;63(2):238–44. doi: 10.1161/HYPERTENSIONAHA.113.02018
Ummee K, Rerkkasem K, Wungrath J. The effect of fluid overload control program on knowledge and behavior among caregivers of end-stage renal disease patients on hemodialysis. Kesmas. 2023;18(4):258–64. doi: 10.21109/kesmas.v18i4.6511
Vanderveen SM, Cohen HW. Sodium intake and mortality follow-up in the Third National Health and Nutrition Examination Survey (NHANES III). J Clin Hypertens (Greenwich). 2009;11(3):85–91. doi: 10.1111/j.1751-7176.2008.00158.x
Wong AT, Munt A, Allman-Farinelli M, Badve SV, Boudville N, Coolican H, et al. Assessment of dietary sodium intake using the scored salt questionnaire in autosomal dominant polycystic kidney disease. Nutrients. 2020;12(11):3376. doi: 10.3390 nu12113376
Kato K, Ishigami T, Kobayashi T, et al. Relationship between changes in blood pressure from summer to winter and estimated 24-hour salt excretion using spot urine: the Niigata Wellness Study. Hypertens Res. 2023;46(1):226–30. doi: 10.1038/s41440-022-01049-1.
Li Y, Zhang P, Wu J, Ma J, Xu J, Zhang X, et al. Twenty-four-hour urinary sodium and potassium excretion and their associations with blood pressure among adults in China: baseline survey of Action on Salt China. Hypertension. 2020;76(5):1580–8. doi: 10.1161/HYPERTENSIONAHA.120.15809
Polit DF, Beck CT. Nursing research: principles and methods. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2004. [24] Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hashimoto T. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16(2):97–103. doi: 10.1038/sj.jhh.1001333
Thai Health Promotion Foundation. NCDs group.[cited 2024 Nov 13]. Available from: https://hpfhub.info/fund-management
Fang K, Li Y, Zhang P, Wu J, Xu J, Zhang X, et al. Dietary sodium intake and food sources among Chinese adults: data from the CNNHS 2010–2012. Nutrients. 2020;12(2):453. doi: 10.3390/nu12020453
Ji Y, Plourde H, Bouzo V, Kilgour RD, Cohen TR. Validity and usability of a smartphone image-based dietary assessment app compared to 3-day food diaries in assessing dietary intake among Canadian adults: randomized controlled trial. JMIR Mhealth Uhealth. 2020;8(9):e16953. doi: 10.2196/16953
Gallani MC, Proulx-Belhumeur A, Almeras N, Després J-P, Doré M, Giguère J-F. Development and validation of a salt food frequency questionnaire (FFQ-Na) and a discretionary salt questionnaire (DSQ) for the evaluation of salt intake among the French-Canadian population. Nutrients. 2020;13(1):105. doi: 10.3390/nu13010105
Gowrishankar M, Blair B, Rieder MJ. Dietary intake of sodium by children: why it matters. Paediatr Child Health. 2020;25(1):47-53. doi: 10.1093/pch/pxz153
Phonsuk P, Vongmongkol V, Satheannoppakao W, Ponguttha S, Prasertsom P, Swinburn BA. Sodium intake and socio-demographic determinants of the non-compliance with daily sodium intake recommendations: Thai NHES IV. J Health Popul Nutr. 2020;39(1):10. doi: 10.1186/s41043-020-00213-1
Department of Health, Ministry of Public Health.Annual report; 2019 [cited 2020 Apr 10]. Available from: https://ihri.org/wp-content/uploads/2020/10/Annual-Report-2019-online.pdf
World Health Organization. WHO global sodium benchmarks for different food categories. [Internet]. Geneva: World Health Organization; 2021. Available from: https://www.who.int/
Sari AN, Farapti F, Md Nor N. Salt taste threshold as a detection of salt intake in hypertensive individuals. JBE. 2022 Sep 26;10(3):227-36. doi: 10.20473/jbe.v10i3.25805
Cohen J. Statistical power analysis. Curr Dir Psychol Sci. 1992;1(3):98-101. doi: 10.1111/1467-8721.ep10768783
DeVellis RF. Scale development: theory and applications. 2nd ed. Thousand Oaks, CA: Sage Publications; 2003.
Fielding CL, Langdon E, et al. Application of the sodium dilution principle to calculate extracellular fluid volume changes in horses during dehydration and rehydration. Am J Vet Res. 2008;69(11):1506-11. doi: 10.2460/ajvr.69.11.1506
Freedman LS, Commins JM, Moler JE, Arab L, Baer DJ, Kipnis V, et al. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for potassium and sodium intake. Am J Epidemiol. 2015;181(7):473-87. doi: 10.1093/aje/kwu325
Laffer CL, Scott RC, Titze JM, Luft FC, Elijovich F. Hemodynamics and salt-and-water balance link sodium storage and vascular dysfunction insaltsensitive subjects. Hypertension. 2016;68(1):195-203. doi:10.1161/HYPERTENSIONAHA.116.07289.
Institute of Nutrition. INMUCAL-Nutrients V2 Program. Nakhon Pathom: Institute of Nutrition, Mahidol University.
Souza DS, Santos BI, Costa BM, Santos DM, Aragão LG, Pires LV, et al. Food frequency questionnaire for foods high in sodium: validation with the triads method. PLoS One. 2023;18(7):e0288123. doi: 10.1371/journal.pone.0288123
Oria M, Yaktine AL, Strom BL, editors. Sodium intake in populations: assessment of evidence. Washington (DC): National Academies Press; 2013.
Sarakarn P, Munpolsri P. Optimal cut-off points for receiver operating characteristic (ROC) curve analysis in developing tools of health innovations: example using Stata. Thai Bull Pharm Sci. 2021;16(1):93-108. doi: 10.69598/tbps.16.1.93-108