Airway clearance techniques for pneumonia patients: A survey of Thai physical therapists
Main Article Content
Abstract
Background: Pneumonia remains a significant global health challenge, necessitating effective management strategies, including airway clearance techniques (ACTs) utilized by physical therapists (PTs).
Objective: This study aims to investigate the selection and usage of ACTs among Thai PTs and examine the influence of work characteristics on these choices.
Materials and methods: A descriptive survey design was employed, targeting licensed PTs in Thailand with at least one year of experience in chest physical therapy. The survey, distributed via online forms and physical therapy units, gathered data on personal demographics, commonly used ACTs, and work characteristics. Out of 178 responses, 137 were included in the study.
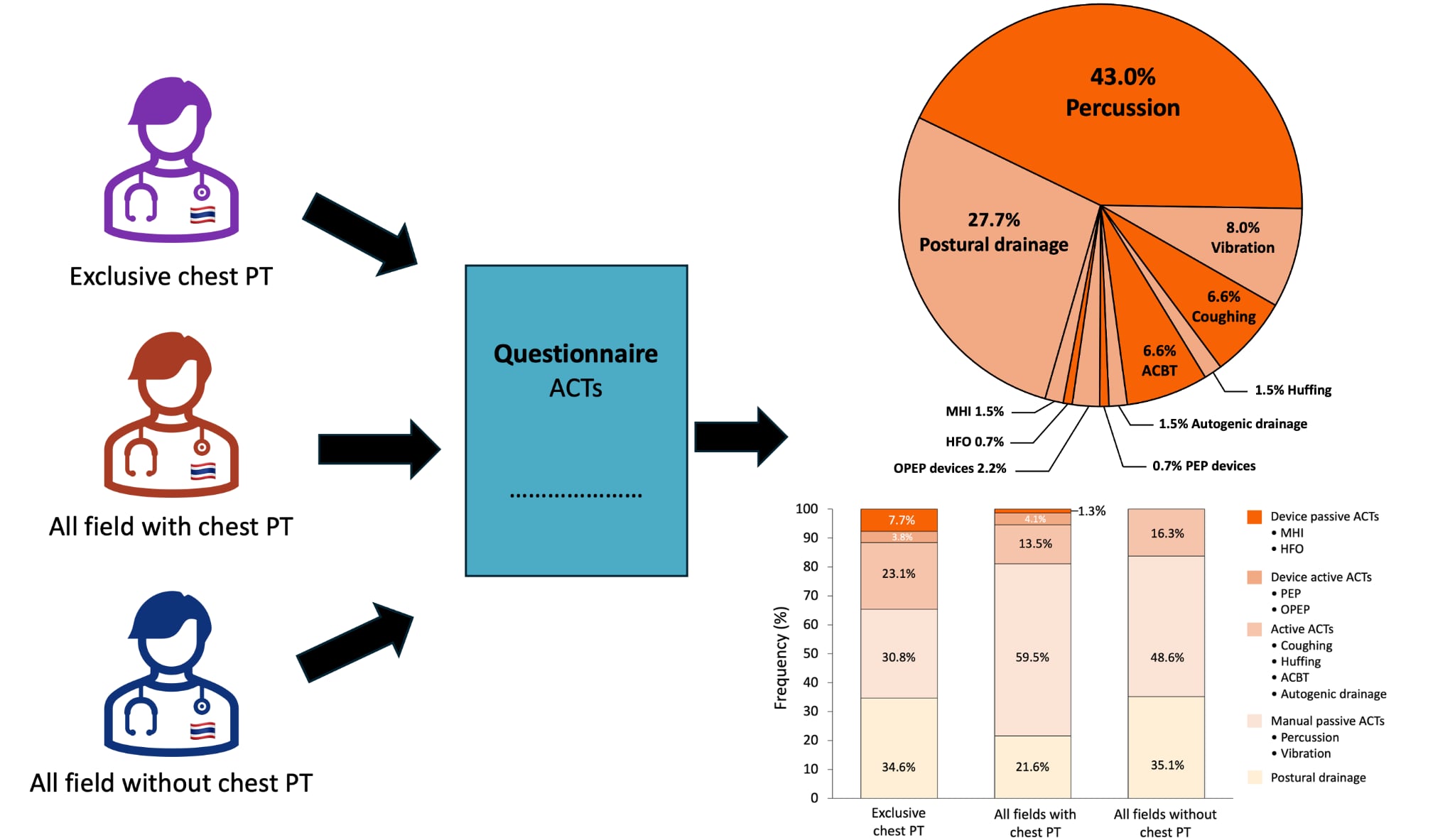
Results: The results indicated a predominant reliance on manual techniques,
particularly percussion and postural drainage, regardless of experience level. However, PTs specializing exclusively in chest physical therapy showed a higher propensity for using advanced techniques and devices such as positive expiratory pressure (PEP) and oscillating positive expiratory pressure (OPEP) devices. The study highlights significant gaps in training and access to advanced airway clearance devices, suggesting a need for targeted continuing education programs.
Conclusion: The findings underscore the importance of promoting a broader range of ACTs in clinical practice to improve patient outcomes. By addressing the barriers to adopting advanced techniques, PTs can enhance their therapeutic interventions and provide more comprehensive care for pneumonia patients. This study provides valuable insights into the current landscape of airway clearance therapy in Thailand, emphasizing the need for improved training and access to necessary equipment to optimize patient care.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. CID. 2007; 44: S27-S72. doi:10.1086/511159.
Chen X, Jiang J, Wang R, Fu H, Lu J, Yang M. Chest physiotherapy for pneumonia in adults. Cochrane Database Syst Rev. 2022; 9:CD006338. PMID:36066373, PMCID: PMC9447368.
Kacmarek RM, Stoller JK, Heuer AJ, Chatburn RL, Kallet RH, editors. Egan’s fundamentals of respiratory care. 12th Edition. St Louis, Missouri: Elsevier; 2021.
Van Der Lee L, Hill A-M, Jacques A, Patman S. Efficacy of Respiratory Physiotherapy Interventions for Intubated and Mechanically Ventilated Adults with Pneumonia: A Systematic Review and Meta-Analysis. Physiother Can. 2021; 73: 6-18. doi:10.3138/ptc-2019-0025.
Physical Therapy Council. Regulations of the Physical Therapy Council Concerning Restrictions and Conditions in the Practice of Physical Therapy, B.E. 2551. 2008. Available: https://pt.or.th/PTCouncil/law/1-2/10.pdf.
Pahal P, Rajasurya V, Sharma S. Typical Bacterial Pneumonia. StatPearls. Treasure Island (FL): Stat-Pearls Publishing; 2023. Available: http://www.ncbi.nlm.nih.gov/books/NBK534295/.
Çakmak A, İnce Dİ, Sağlam M, Savcı S, Yağlı NV, Kütükcü EÇ, et al. Physiotherapy and rehabilitation implementation in intensive care units: A Survey Study. Turk Thorac J. 2019; 20: 114-9. doi: 10.5152/TurkThoracJ.2018.18107.
Audsavachulamanee B, Aueyingsak S, Ubolsaka-Jones C, Kosura N, Chanapon J, Yubonpan N, et al. Thai physiotherapists’ performance of manual chest wall percussion on an artificial lung: frequency, force, and fatigue perception. Arch AHS. 2023; 35: 23-34.
Audsavachulamanee B, Nwe AA, Ubolsaka-Jones C, Kosura N, Hongratana G, Aueyingsak S, et al. The flow-pressure and cardiopulmonary responses of manual chest percussion with different ranges of oscillation frequency in healthy subjects. Trends Sci.2024; 21: 7345. doi:10.48048/tis.2024.7345.
Audsavachulamanee B, Aueyingsak S, Ubolsakka-Jones C, Bansri A, Chaiyasang J, Srilasalai S, et al. Physiotherapist performance during manual chest vibration in simulated adult lung: frequency, force and pattern. Asia Pac J Sci Technol. 2024; 29(3): 14-21. doi:10.14456/apst.2024.48.
Paz JC, West MP. Acute care handbook for physical therapists. 4th Edition. St. Louis, Missouri: Elsevier Saunders; 2014.
Langenderfer B. Alternatives to percussion and postural drainage. A review of mucus clearance therapies: percussion and postural drainage, autogenic drainage, positive expiratory pressure, flutter valve, intrapulmonary percussive ventilation, and high-frequency chest compression with the ThAIRapy Vest. J Cardiopulm Rehabil. 1998; 18: 283-9. doi: 10.1097/00008483-199807000-00005.
Van Der Lee L, Hill A, Patman S. Expert consensus for respiratory physiotherapy management of mechanically ventilated adults with community-acquired pneumonia: A D elphi study. J Eval Clin Pract. 2019; 25: 230-43. doi: 10.1111/jep.13077.
Mckoy NA, Wilson LM, Saldanha IJ, Odelola OA, Robinson KA. Active cycle of breathing technique for cystic fibrosis. Cochrane Database Syst Rev. 2016; 7: CD007862. doi:10.1002/14651858.CD007862.pub4.
Kwan BPM, Hill A-M, Elliott M, Van Der Lee L. A retrospective study of physiotherapy management for patients with pneumonia requiring invasive ventilation in a single-center Australian ICU. Hong Kong Physiother J. 2022; 42: 55-64. doi: 10.1142/S1013702522500068.
Van Der Lee L, Patman S, Hill A-M. Development of a clinical practice guideline for physiotherapy management of adults invasively ventilated with community-acquired pneumonia. Physiotherapy. 2024; 122: 57-67. doi: 10.1016/j.physio.2023.12.003.
C. Phimphasak et al. Journal of Associated Medical Sciences 2025; 58(3): 122-128128
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. The Lancet. 2009; 373: 1874-82. doi:10.1016/S0140-6736(09)60658-9.
Larsen T, Lee A, Brooks D, Michieli S, Robson M, Veens J, et al. Effect of early mobility as a physiotherapy treatment for pneumonia: A systematic review and meta-analysis. Physiother Can. 2019; 71: 82-9. doi:10.3138/ptc.2017-51.ep.
Van Der Lee L, Hill A-M, Patman S. After-hours respiratory physiotherapy for intubated and mechanically ventilated patients with community-acquired pneumonia: An Australian perspective. Aust Crit Care. 2018; 31: 349-54. doi: 10.1016/j.aucc.2017.10.001.