The reference intervals for biochemistry analytes obtained through the indirect method indicate the metabolic shifts in the Thai adult population
Main Article Content
Abstract
Background: Reference intervals (RIs) of biochemistry analytes are required to make medical decisions. According to the standards, medical laboratories shall validate and/or verify RI for their own uses because there are biological and laboratory variations.
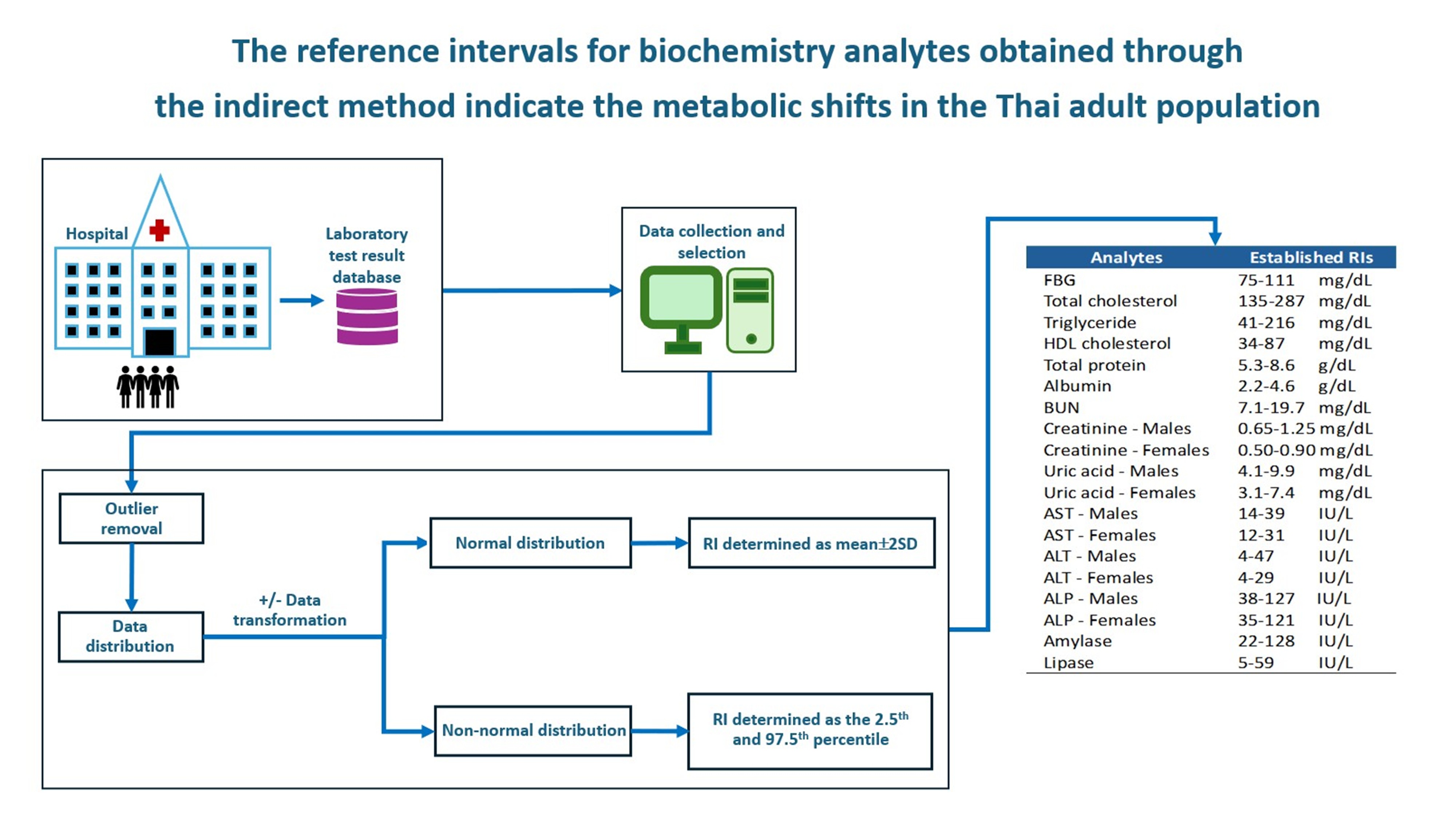
Objective: To determine RIs of 14 biochemistry analytes, including fasting blood glucose, total cholesterol, HDL cholesterol, triglyceride, total protein, albumin, BUN, creatinine, uric acid, AST, ALT, ALP, amylase, and lipase in Thai adults.
Materials and methods: RIs were determined by using the indirect method. Test results from 18 years old or older out-patient department patients were collected from the hospital laboratory database from January 2019 to December 2021. The results from subjects with a high likelihood of disease were excluded, outliers were removed, data distribution was tested, and RIs were determined as either mean±2SD or the 2.5th to 97.5th percentile for normal and non-normal distribution data, respectively.
Results: There were 197,897 test results available for RI determination. Most of the determined RIs were comparable to those from the manufacturer, except uric acid. All 14 RIs passed verification criteria in the population served. Interestingly, our RIs for blood total cholesterol, triglyceride, and uric acid were higher than those established in the previous reports in Thai population.
Conclusion: The RIs were established and verified in Thai adults; therefore, they could be implemented for the population. In addition, our RIs of total cholesterol, triglyceride, and uric acid reflect metabolic changes of the studied population.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Doyle K, Bunch DR. Reference intervals: past, present, and future. Crit Rev Clin Lab Sci. 2023; 60(6): 466-82. doi: 10.1080/10408363.2023.2196746.
Horowitz GL, Altaie S, Boyd JC. Defining, establishing, and verifying reference intervals in the clinical laboratory; approved guideline: CLSI; 2010.
Xu P, Zhou Q, Xu J. Reference interval transference of common clinical biomarkers. Scand J Clin Lab Invest. 2021; 81(4): 264-71. doi: 10.1080/00365513.2021.1907858.
Badrick T. Biological variation: Understanding why it is so important? Pract Lab Med. 2021; 23: e00199. doi: 10.1016/j.plabm.2020.e00199.
Jones GRD, Haeckel R, Loh TP, Sikaris K, Streichert T, Katayev A, et al. Indirect methods for reference interval determination - review and recommendations. Clin Chem Lab Med. 2018; 57(1): 20-9. doi: 10.1515/cclm-2018-0073.
Katayev A, Balciza C, Seccombe DW. Establishing reference intervals for clinical laboratory test results: is there a better way? Am J Clin Pathol. 2010; 133(2): 180-6. doi: 10.1309/AJCPN5BMTSF1CDYP.
Özcürümez MK, Haeckel R, Gurr E, Streichert T, Sack U. Determination and verification of reference interval limits in clinical chemistry. Recommendations for laboratories on behalf of the working group guide limits of the DGKL with respect to ISO Standard 15189 and the Guideline of the German Medical Association on Quality Assurance in Medical Laboratory Examinations (Rili-BAEK). J Lab Med. 2019; 43(3): 127-33. doi: 10.1515/labmed-2018-0500.
Ozarda Y. Establishing and using reference intervals. Turk J Biochem. 2020; 45(1): 1-10. doi: 10.1515/tjb-2017-0299.
Wang QP, Guo LY, Lu ZY, Gu JW. Reference intervals established using indirect method for serum ferritin assayed on Abbott Architect i2000(SR) analyzer in Chinese adults. J Clin Lab Anal. 2020; 34(3): e23083. doi: 10.1002/jcla.23083.
Tukey JW. Exploratory data analysis. Addison-Wesley Publishing; 1977.
Ozarda Y, Higgins V, Adeli K. Verification of reference intervals in routine clinical laboratories: practical challenges and recommendations. Clin Chem Lab Med. 2019; 57(1): 30-7. doi: 10.1515/cclm-2018-0059.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106(25): 3143-421.
Viriyayudhakorn S, Mitarnun W, Pornpatkul M, Jenjareontham R, Khoprasert B, Ruangrairatanaroje P, et al. Reference intervals of twenty-one biochemical constituents of the population in southern Thailand. J Med Assoc Thailand. 1983; 66(10): 579-89.
Chamnanpai S, Charuruks N, Watanaboonyoungcharoen P, Kalayanachati A. Reference intervals of clinical chemistry parameters in adults at King Chulalongkorn Memorial Hospital. Chula Med J. 2004; 48(8). doi: 10.58837/CHULA.CMJ.48.8.3.
Yotsakullert C, Klongkayan A, Wongwattanakul M, Daduang J, Jearanaikoon P, Tippayawat P. Clinical chemistry normal ranges of healthy adult population in Nong Khai, Thailand. Arch AHS. 2020; 32(3): 1-12.
Chatchawal P, Wongwattanakul M, Thubthimngam C, Yotsakullert C, Jearanaikoon P. Establishment of reference intervals in biochemistry parameters from check-up records: AMS Medical Laboratory, Khon Kaen. Asia Pac J Sci Technol. 2023; 29(01): APST-29. doi: 10.14456/apst.2024.5
Enkhmaa B, Surampudi P, Erdembileg A. Lifestyle changes: Effect of diet, exercise, functional Food and obesity treatment on lipids and lipoproteins. 2015.
Kopp W. How Western diet and lifestyle drive the pandemic of obesity and civilization diseases. Diabetes Metab Syndr Obes 2019; 12: 2221-36. doi: 10.2147/DMSO.S216791.
Bovolini A, Garcia J, Andrade MA, Duarte JA. Metabolic Syndrome Pathophysiology and Predisposing Factors. Int J Sports Med. 2021; 42(3): 199-214. doi: 10.1055/a-1263-0898.
Zhubi-Bakija F, Bajraktari G, Bytyçi I, Mikhailidis DP, Henein MY, Latkovskis G, et al. The impact of type of dietary protein, animal versus vegetable, in modifying cardiometabolic risk factors: A position paper from the International Lipid Expert Panel (ILEP). Clin Nutr. 2021; 40(1): 255-76. doi: 10.1016/j.clnu.2020.05.017.
Wen ZY, Wei YF, Sun YH, Ji WP. Dietary pattern and risk of hyperuricemia: an updated systematic review and meta-analysis of observational studies. Front Nutr. 2024; 11: 1218912. doi: 10.3389/fnut.2024.1218912.
Ekpenyong CE, Daniel N. Roles of diets and dietary factors in the pathogenesis, management and prevention of abnormal serum uric acid levels. PharmaNutrition. 2015; 3(2): 29-45. doi: 10.1016/j.phanu.2014.12.001.
Johnson RJ, Nakagawa T, Sanchez-Lozada LG, Shafiu M, Sundaram S, Le M, et al. Sugar, uric acid, and the etiology of diabetes and obesity. Diabetes. 2013; 62(10): 3307-15. doi: 10.2337/db12-1814.
Klongthalay S, Suriyaprom K. Increased uric acid and lifestyle factors associated with metabolic syndrome in Thais. Ethiop J Health Sci. 2020; 30(2): 199-208. doi: 10.4314/ejhs.v30i2.7.
Fahed G, Aoun L, Bou Zerdan M, Allam S, Bou Zerdan M, Bouferraa Y, et al. Metabolic syndrome: Updates on pathophysiology and management in 2021. Int J Mol Sci. 2022; 23(2). 786. doi: 10.3390/ijms23020786.
Maloberti A, Tognola C, Garofani I, Algeri M, Shkodra A, Bellantonio V, et al. Uric acid and metabolic syndrome: Importance of hyperuricemia cut-off. Int J Cardiol. 2024; 417: 132527. doi: 10.1016/j.ijcard.2024.132527.
Le Boedec K. Reference interval estimation of small sample sizes: A methodologic comparison using a computer-simulation study. Vet Clin Pathol. 2019; 48(2): 335-46. doi: 10.1111/vcp.12725.