Translation, cross-cultural adaptation and psychometric properties of the Thai version of the Trunk Control Measurement Scale for children with cerebral palsy
Main Article Content
Abstract
Background: Trunk impairment is an important clinical feature in children with cerebral palsy (CP), therefore assessment of trunk control is a crucial part of functional assessment in children with CP.
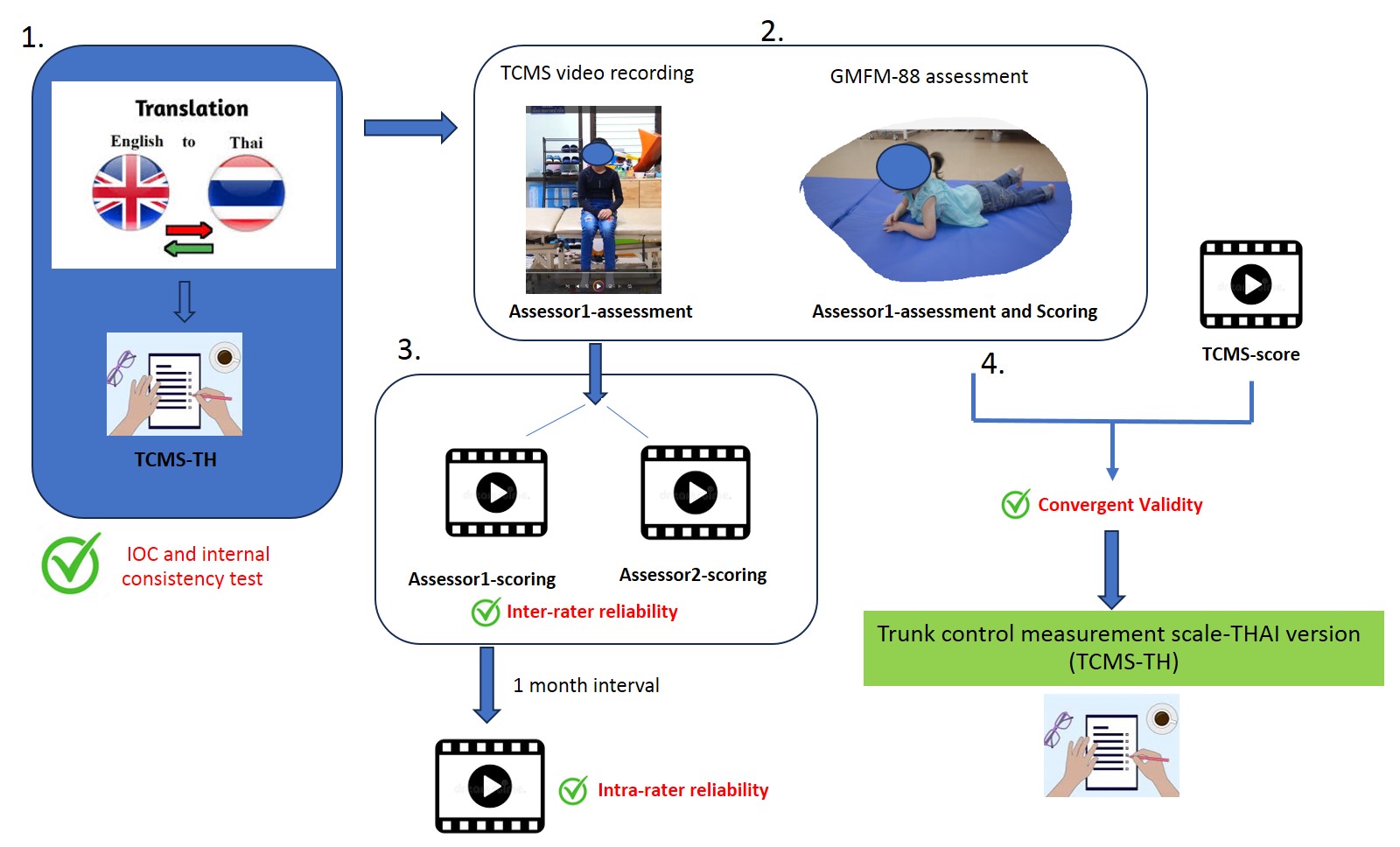
Objectives: The study aimed to translate the Trunk Control Measurement Scale (TCMS) from the original English into a Thai version and demonstrate the reliability and validity of the TCMS-TH among children with spastic CP.
Materials and methods: The TCMS was translated using standard cross-cultural adaptation guidelines. The final TCMS-TH was tested on 29 children with spastic CP aged 5-15 years. For inter-rater reliability, two assessors independently scored the children from the video recording using the TCMS-TH. One month after the first assessment, a second assessment was performed to determine intra-rater reliability. The convergent validity of the TCMS-TH was assessed by comparison to the Gross Motor Function Measure (GMFM-88). The intraclass correlation coefficient (ICC) and Pearson’s correlation coefficient were used to analyze reliability and validity.
Results: The TCMS-TH had good internal consistency, with Cronbach’s alpha = 0.916 for the total TCMS-TH. Inter-rater reliability was good to excellent, ICC = 0.837-0.955, whereas intra-rater reliability was excellent, ICC =0.918-0.995. The TCMS-TH and the GMFM has moderate to high correlation (r=0.631-0.810).
Conclusion: The TCMS-TH is a reliable and valid tool for assessing trunk control in children with spastic CP. However, its outcomes are primarily generalizable to observations obtained from video recordings rather than direct in-person assessments. Despite this limitation, the TCMS-TH remains a valuable tool for both clinical practice and research settings.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Armstrong RW. Definition and classification of cerebral palsy. Dev Med Child Neurol. 2007; 49(3): 166. doi: 10.1111/j.1469-8749.2007.00166.x.
Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, Dan B, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005; 47(8): 571-6. doi: 10.1017/s001216220500112x.
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007; 109: 8-14. doi:10.1111/j14699-8749.2007.tb12610.x.
Carlberg EB, Hadders-Algra M. Postural dysfunction in children with cerebral palsy: some implications for therapeutic guidance. Neural Plast. 2005;12:221-8.
Rose J, Wolff DR, Jones VK, Bloch DA, Oehlert JW, Gamble JG. Postural balance in children with cerebral palsy. Dev Med Child Neurol. 2002; 44(1): 58-63. doi: 10.1017/s0012162201001669.
Reid DT. The effects of the saddle seat on seated postural control and upper-extremity movement in children with cerebral palsy. Dev Med Child Neurol. 1996; 38(9): 805-15. doi: 10.1111/j.1469-8749.1996.tb15115.x.
Rachwani J, Santamaria V, Saavedra SL, Woollacott MH. The development of trunk control and its relation to reaching in infancy: a longitudinal study. Front Hum Neurosci. 2015; 9:94. doi: 10.3389/fnhum.2015.00094.
Heyrman L, Desloovere K, Molenaers G, Verheyden G, Klingels K, Monbaliu E, et al. Clinical characteristics of impaired trunk control in children with spastic cerebral palsy. Res Dev Disabil. 2013; 34: 327-34. doi: 10.1016/j.ridd.2012.08.015.
Liao SF, Yang TF, Hsu TC, Chan RC, Wei TS. Differences in seated postural control in children with spastic cerebral palsy and children who are typically developing. Am J Phys Med Rehabil. 2003; 82(8): 622-6. doi: 10.1097/01.PHM.0000073817.51377.51.
Donker SF, Ledebt A, Roerdink M, Savelsbergh GJ, Beek PJ. Children with cerebral palsy exhibit greater and more regular postural sway than typically developing children. Exp Brain Res. 2008; 184(3): 363-70. doi: 10.1007/s00221-007-1105-y.
Heyrman L, Feys H, Molenaers G, Jaspers E, Monari D, Nieuwenhuys A, et al. Altered trunk movements during gait in children with spastic diplegia: compensatory or underlying trunk control deficit? Res Dev Disabil. 2014; 35(9): 2044-52. doi: 10.1016/j.ridd.2014.04.031.
Montero Mendoza S, Gomez-Conesa A, Hidalgo Montesinos MD. Association between gross motor function and postural control in sitting in children with Cerebral Palsy: a correlational study in Spain. BMC pediatr. 2015; 15: 124. doi: 10.1186/s12887-015-0442-4.
Nordmark E, Hägglund G, Jarnlo GB. Reliability of the gross motor function measure in cerebral palsy. Scand J Rehabil Med. 1997;29(1):25-8.
Lundkvist Josenby A, Jarnlo GB, Gummesson C, Nordmark E. Longitudinal construct validity of the GMFM-88 total score and goal total score and the GMFM-66 score in a 5-year follow-up study. Phys Ther. 2009; 89(4): 342-50. doi: 10.2522/ptj.20080037.
Butler PB, Saavedra S, Sofranac M, Jarvis SE, Woollacott MH. Refinement, reliability, and validity of the segmental assessment of trunk control. Pediatr Phys Ther. 2010; 22(3): 246-57. doi: 10.1097/PEP.0b013e3181e69490.
Hansen L, Erhardsen KT, Bencke J, Magnusson SP, Curtis DJ. The Reliability of the Segmental Assessment of Trunk Control (SATCo) in Children with Cerebral Palsy. Phys Occup Ther Pediatr. 2018; 38(3): 291-304. doi: 10.1080/01942638.2017.1337662.
Heyrman L, Molenaers G, Desloovere K, Verheyden G, De Cat J, Monbaliu E, et al. A clinical tool to measure trunk control in children with cerebral palsy: the Trunk Control Measurement Scale. Res Dev Disabil. 2011; 32(6): 2624-35. doi: 10.1016/j.ridd.2011.06.012.
Verheyden G, Nieuwboer A, Mertin J, Preger R, Kiekens C, De Weerdt W. The Trunk Impairment Scale: a new tool to measure motor impairment of the trunk after stroke. Clin Rehabil. 2004; 18(3): 326-34. doi: 10.1191/0269215504cr733oa.
Jeon JY, Shin WS. Reliability and validity of the Korean version of the trunk control measurement scale (TCMS-K) for children with cerebral palsy. Res Dev Disabil. 2014; 35(3): 581-90. doi: 10.1016/j.ridd.2014.01.009.
Mitteregger E, Marsico P, Balzer J, van Hedel HJA. Translation and construct validity of the Trunk Control Measurement Scale in children and youths with brain lesions. Res Dev Disabil. 2015; 45-46: 343-52. doi: 10.1016/j.ridd.2015.08.007.
Lopez J, Estrada C, Gomez C, Egea-Gámez R, Valera Calero J, Casas P, et al. Trunk Control Measurement Scale (TCMS): Psychometric Properties of Cross-Cultural Adaptation and Validation of the Spanish Version. Int J Environ Res Public Health. 2023; 20: 5144. doi: 10.3390/ijerph20065144.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000; 25(24): 3186-91. doi: 10.1097/00007632-200012150-00014.
Turner R, Carlson L. Indexes of Item-Objective Congruence for Multidimensional Items. Int J Test. 2003; 3: 163-71. doi: 10.1207/S15327574IJT0302_5.
Ko J, Kim M. Reliability and responsiveness of the gross motor function measure-88 in children with cerebral palsy. Physical therapy. 2013; 93(3): 393-400. doi: 10.2522/ptj.20110374.
Weis R. Gross Motor Function Measure (GMFM-66 and GMFM-88) User’s Manual. J Paediatr Neurol. 2004; 8: 111-2. doi: 10.1016/j.ejpn.2003.11.003.
Domholdt E. Physical Therapy Research : Principles and Applications. Philadelphia [Pennsylvania]: W.B. Saunders Company; 2000.
Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012; 24(3): 69-71.
Choi Y-E, Jung H-R, Kim J-H. Comparison of Trunk Control on Gross Motor Function and Topography in Children with Spastic Cerebral Palsy. J Korean Soc of Phys Med. 2019; 14: 45-53. doi: 10.13066/kspm.2019.14.4.45.
Keeratisiroj O, Thawinchai N, Siritaratiwat W, Buntragulpoontawee M. Prognostic Predictors for Ambulation in Thai Children With Cerebral Palsy Aged 2 to 18 Years. J. Child Neurol. 2015; 30: 1812-8. doi: 10.1177/0883073815582267.