Integrated long-term care model for dependent elderly in Mahasarakham Province, Thailand
Main Article Content
Abstract
Background: Long-term care (LTC) for dependent elderly individuals encompasses a wide range of medical, personal, and social services designed to meet their physical, emotional, and psychological needs over an extended period.
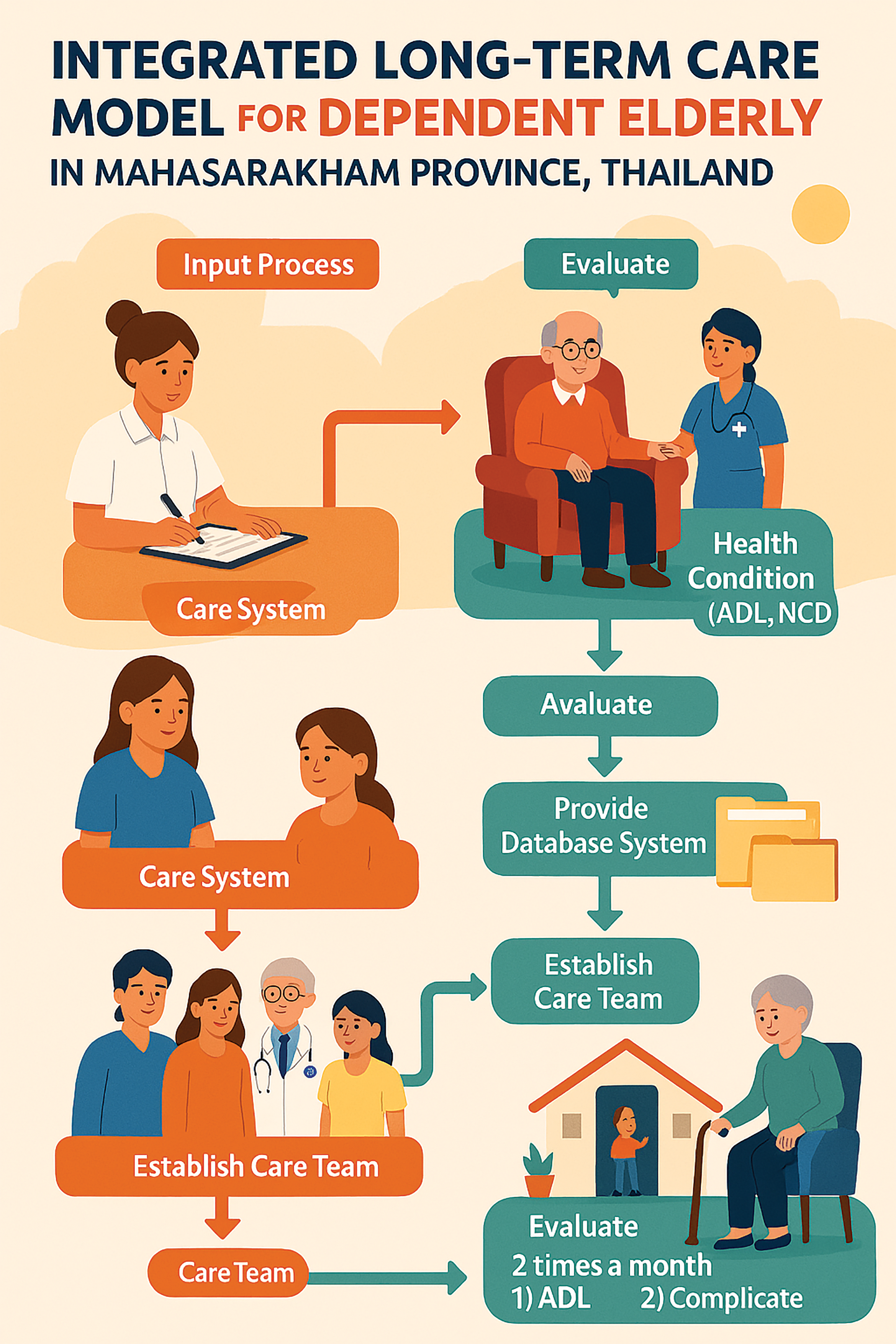
Objective: This study aimed to develop and evaluate an integrated long-term care model for dependent elderly individuals in Mahasarakham Province.
Materials and methods: A mixed-methods research design divided into three phases: Phase 1 focused on identifying the problems and care needs of dependent elderly individuals; Phase 2 involved the development of an integrated care model; and Phase 3 involved the implementation and evaluation of the model. The Geographic Information Systems (GIS) application was crucial for identifying where care support was needed. The study included 95 elderly participants and seven caregivers. Data was collected using questionnaires and structured interviews.
Results: The study included 60% female and 40% male participants, with the majority (34.74%) falling within the age more than 75 years. Hypertension was as the most prevalent underlying condition, affecting 42.11% of the sample. In terms of elderly dependency, 8.42% of participants were severe dependency, while 6.32% were deemed completely dependent. The Barthel ADL Index analysis showed that the average score for daily living activities before care was 6.56 (with a standard deviation of 4.64), and this score went up to 10.22 (with a standard deviation of 8.19) after receiving care. Additionally, caregivers’ knowledge regarding elderly dependency care showed significant improvement following a structured training program. The mean score of caregiver knowledge increased after the training, with the change being statistically significant.
Conclusion: This model highlights its potential for broader application, offering a promising approach to improving the quality of life for the elderly by enhancing their ability to perform ADL activities. By integrating this program into local and regional healthcare strategies, it will contribute to the overall healthcare campaign, fostering improved health outcomes and a higher quality of life for dependent elderly people.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
United Nations. World population prospects 2022: Summary tables [Internet]. 2022 [cited 2024 Dec 6]. Available from: https://www.un-ilibrary.org/content/ books/9789210014380/read.
World Health Organization. Global report on aging and health. Geneva: WHO; 2021.
Department of Older Persons. Situation of the Thai Older Persons 2023. Bangkok: Amarin Corporations Public Company Limited; 2023.
Foundation of Thai Gerontology Research and Development Institute. Situation of the Thai elderly 2020. Bangkok: FTGRDI; 2020.
Ministry of Public Health. Health Region 7 Annual Report 2024. Bangkok: MOPH; 2024.
Provincial Health Office of Maha Sarakham. Elderly population report 2024. Maha Sarakham: PHO; 2024.
Deming WE. Out of the crisis. Cambridge: MIT Center for Advanced Educational Services; 1986.
Department of Medical Services, Ministry of Public Health. Guidelines for Screening and Health Assessment of the Elderly, B.E. 2564 (2021). Nonthaburi: Ministry of Public Health; 2021.
Pongratanakul R, Thitisakulchai P, Srinonprasert V, Siriussawakul A, Suraarunsumrit P, Dajpratham P. Development and Psychometric Evaluation of a Short- Form Barthel Index for Older Patients Undergoing Abdominal Surgery. ASEAN J Rehabil Med [internet]. 2023 Sep. 25 [cited 2025 May 9]; 33(3): 135. available from: https://he01.tci-thaijo.org/index.php/aseanjrm/ article/view/262902.
Chen TL, Feng YH, Kao SL, Lu JW, Loh CH. Impact of integrated health care on the elderly population: A systematic review of Taiwan’s experience. Arch Gerontol Geriatr. 2022; 102: 1-9. doi: 10.1016/j.archger. 2022.104746.
Li Y, Luo L, Dong H. Delivering integrated community care for the elderly: A qualitative case study in Southern China. Int J Environ Res Public Health. 2024; 21(6): 1-17. doi: 10.3390/ijerph21060680.
Heggdal K, Mendelsohn JB, Stepanian N, Oftedal BF, Larsen MH. Health-care professionals’ assessment of a person-centred intervention to empower self- management and health across chronic illness: Qualitative findings from a process evaluation study. Health Expect. 2021; 24(6): 1367-77. doi: 10.1111/ hex.13271.
Liljas, AEM, et al. Impact of Integrated Care on Patient- Related Outcomes Among Older People – A Systematic Review. International Journal of Integrated Care, 2019; 19(3): 1-16. doi: 10.5334/ijic.4632.
Pedersen AKB, Skinner MS, Sogstad M. Needs assessment in long-term care: Expression of national principles for priority setting in service allocation. BMC Health Serv Res. 2024; 24(530): 1-11. doi: 10.1186/ s12913-024-10889-1.
Takeda C, Guyonnet S, Sumi Y, Vellas B, Araujo de Carvalho I. Integrated care for older people and the implementation in the INSPIRE care cohort. J Prev Alzheimers Dis. 2020; 7(2): 70-4. doi: 10.14283/jpad. 2020.8.
Fulmer T, Mate KS, Berman A. The age-friendly health system imperative. J Am Geriatr Soc. 2018; 66(1): 22-4. doi: 10.1111/jgs.15076.
Chang KT. Introduction to geographic information systems. New York: McGraw-Hill; 2008.
World Health Organization. World report on ageing and health. WHO Press; 2015. Available from: https:// www.who.int/publications/i/item/9789241565042.
Kane RL, Kane RA. Assessing older persons: Measures, meaning, and practical applications. Oxford University Press; 2018.