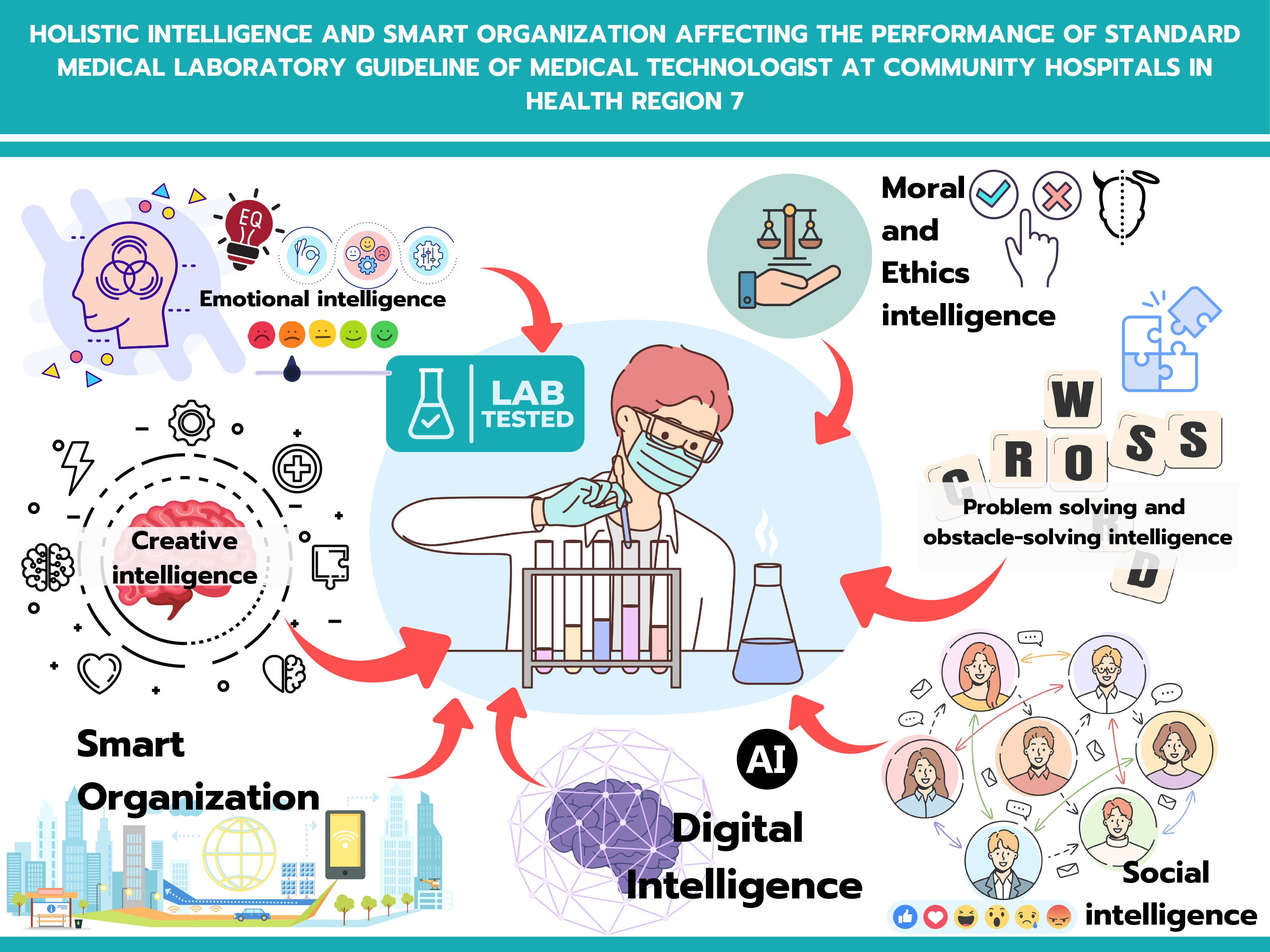
Holistic intelligence and smart organization affecting the performance of standard medical laboratory guidelines of medical technologists at community hospitals in Health Region 7
Main Article Content
Abstract
Background: Medical laboratories are vital components of healthcare systems in community hospitals, serving as frontline facilities in public healthcare. The development of laboratory quality standards requires comprehensive improvement in personnel and organizational aspects to ensure public confidence and safety in service delivery.
Objective: This cross-sectional descriptive research aimed to study the effects of holistic intelligence and intelligent organization on medical laboratory standard practices among medical technologists in community hospitals within Health Region 7.
Materials and methods: The sample consisted of 187 medical technologists from community hospitals in Health Region 7, selected through stratified random sampling proportionally by province, followed by simple random sampling within each province. Data were collected between November 13-23, 2024, using an online questionnaire validated for content by three experts, with an overall reliability coefficient of 0.988. Data analysis employed descriptive statistics, Pearson’s correlation coefficient, and stepwise multiple linear regression.
Results: The results revealed that overall holistic intelligence was at a high level (Mean=4.12, SD=0.45), overall intelligent organization was at a high level (Mean=3.80, SD=0.65), and overall adherence to medical laboratory standards was at a high level (Mean=4.27, SD=0.49). Both holistic intelligence and intelligent organization showed statistically significant moderate positive correlations with medical laboratory standard practices (r=0.599, p<0.001 and r=0.557,><0.001 and r=0.557, p<0.001 and r=0.557,><0.001, respectively). Predictive factor analysis identified organizational learning system co-creation (B=0.266), moral and ethical intelligence (B=0.262), and emotional intelligence (B=0.213) as significant predictors, collectively explaining 47.2% of the variance in medical laboratory standard practices (R²adj=0.472).
Conclusion: Based on these findings, relevant agencies should develop organizational learning systems through the establishment of learning centers and mentoring systems, enhance moral and ethical intelligence through training and knowledge exchange, and improve personnel emotional management skills to elevate the quality and safety standards of medical laboratory operations in community hospitals.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
National Economic and Social Development Council. The 20-Year National Strategy (2018-2037). Bangkok: Office of the PrimeMinister; [Internet]2022. [Cited 2024 May 20]. Available from https://www.nesdc. go.th/download/document/SAC/NS_SumPlanOct 2018.pdf (in Thai)
Department of Medical Sciences Medical Laboratory Standards Nonthaburi: Ministry of Public Health; 2019. (in Thai)
Goleman D. Working with emotional intelligence. New York: Bantam Books; 1998.
Lennick D Kiel F. Moral intelligence: enhancing business performance and leadership success. New Jersey: Pearson Education; 2011.
Stoltz PG. Adversity quotient: turning obstacles into opportunities. New York: John Wiley and Sons; 1997.
Albrecht K. Social intelligence: the new science of success. San Francisco: Jossey-Bass A Wiley Imprint; 2006.
Torrance EP. Teaching for creativity. In: Isaksen SG, Ed. Frontiers of creativity research: beyond the basics. Buffalo, NY: Bearly Limited; 1987. p.189-215.
Park Y. DQ Global Standards Report 2019 Common Framework for Digital Literacy, Skills and Readiness. DQ Institute. [Internet] [Cited 2024 June 8]. Available from https://www.dqinstitute.org/wpcontent/uploads/ 2019/03/DQ%20Global%20Standards%20Report 2019.pdf
Siriraj Hospital. SMART Organization. Siriraj Public Relations Journal 2018; 30(408):18. (in Thai).
Health Region 7 Office. Medical Technologist Data in Health Region 7, Fiscal Year 2024. Khon Kaen: Situation Report of Health Region 7; 2024. (in Thai)
Bureau of Laboratory Quality Standards. List of medical laboratories accredited to the medical laboratory standards, [Internet] [Cited 2024 May 20]. Available from https://blqs.dmsc.moph.go.th/pageview/522 (in Thai)
The Medical Technology Council of Thailand. List of laboratory quality accreditation. [Internet] [Cited 2024 May 20]. Available from https://mtcouncil.org/ lab-quality-accreditation/ (in Thai)
Thipat S, Ratsameetes B. Factors affecting laboratory accreditation in Army hospitals. Royal Thai Army Med J. 2015; 68(2): 61-9.(document (9)). (in Thai)
Artittaya Piatanom, Youwanuch Sattayasomboon, Bhusita Intaraprasong, Jutatip Sillabutra. Work Related Quality of Life among Medical Technologists in Regional Hospital, Ministry of Public Health. Journal of Health Science. 2022; 31(1): 144-53. (in Thai).
Cohen J. Statistical power analysis for the behavior sciences (2nd Ed.). Hillsdale, NJ: Lawrence Erlbaum; 1988.
Anut Wattana, Prachak Bouphan, Surachai Phimha. Personal Characteristics and Leadership Soft Skills Affecting Physical Therapist Performance in Heath Region 8. Journal of Health Science and Community Public Health.2024; 7(1): 84-95. (in Thai).
Thompson SK. Sampling. 3rd Ed. New York: John Wiley & Sons; 2012.
Likert R. The human organization: Its management and values. New York: McGraw-Hill; 1967.
Chansuwan S, Buathuan S. Social science research methodology. Khon Kaen: Department of Sociology and Anthropology, Faculty of Humanities and Social Sciences, Khon Kaen University; 2004. (in Thai)
Elifson KW, Runyon RP, Haber A. Fundamentals of social statistics. 2nd Ed. New York: McGraw-Hill; 1990.
Siritunyanont R, Chamdit S, Wongyot B. Establishing a quality certification system for diagnostic radiology laboratory in Thailand. J Health Syst Res. 2024; 18(2): 220-38(hsri-journal-v18n2-p220). (in Thai).
Muenphon S, Sroisangwan P, Wongwanich S, Ladiyood N. Development program for Thai medical laboratories for ISO 15189. J Med Sci Dep Med Sci. 2021; 63(1): 119-34.(in Thai).
Wilson ML, Fleming KA, Kuti MA, Looi LM, Lago N, Ru K. Access to pathology and laboratory medicine services: a crucial gap. The Lancet. 2018; 391(10133): 1927-38. doi: 10.1016/S0140-6736(18)30458-6.
Karen, J.F., Jiju, A., & Alex, D. Critical success factors of continuous improvement in the public sector. The TQM Magazine. 2007; 19(5): 497-517. doi: 10.1108/09544780710817900
Panchapakesan, P., Rajendran, C., & Sai, L.P. A conceptual framework of service quality in healthcare. Benchmarking: An International Journal, 2009; 16(2): 157-91. doi:10.1108/14635770910948213
Sakr, F., Haddad, C., Zeenny, R. M., et al. Work Ethics and Ethical Attitudes among Healthcare Professionals: The Role of Leadership Skills in Determining Ethics Construct and Professional Behaviors. Healthcare, 2022; 10(8): 1399. doi:10.3390/healthcare10081399
Al-Adamat, A., Al-Gasawneh, J., & Al-Adamat, O. The impact of moral intelligence on green purchase intention. Management Science Letter. 2020; 10(9): 2063-70. doi:10.5267/j.msl.2020.2.005
Khoshmehr, Z., Barkhordari-Sharifabad, M., Nasiriani, K., & Fallahzadeh, H. Moral courage and psychological empowerment among nurses. BMC Nursing, 2020; 19(1): 1-7. doi: 10.1186/s12912-020-00435-9
Mehralian, G., Bordbar, S., Bahmaei, J., Askarpour, H., & Yusefi, A. R. The impact of emotional and moral intelligence on nurses’ organizational commitment. BMC Nursing, 2024; 23(1): 1-13. doi:10.1186/s12912- 024-02455-1
Karimi, L., Leggat, S. G., Bartram, T., & Rada, J. The effects of emotional intelligence training on the job performance of Australian aged care workers. Health Care Management Review. 2020; 45(1): 41-51. doi:10.1097/HMR.0000000000000200
Meng, L., & Qi, J. The effect of an emotional intelligence intervention on reducing stress and improving communication skills of nursing students. NeuroQuantology. 2018; 16(1): 1-9. doi:10.14704/nq.2018. 16.1.1175
Tawfik, D. S., Scheid, A., Profit, J., Shanafelt, T., Trockel, M., Adair, K. C., et al. Evidence relating health care provider burnout and quality of care: A systematic review and meta-analysis. Annals of Internal Medicine. 2019; 171(8): 555-67. doi: 10.7326/M19-1152.
O’Connor, P. J., Hill, A., Kaya, M., & Martin, B. The measurement of emotional intelligence: A critical review of the literature and recommendations for researchers and practitioners. Frontiers in Psychology. 2019; 10: 1116. doi:10.3389/fpsyg.2019.01116