Core stabilization exercise can improve lumbar joint position sense in healthy individuals
Main Article Content
Abstract
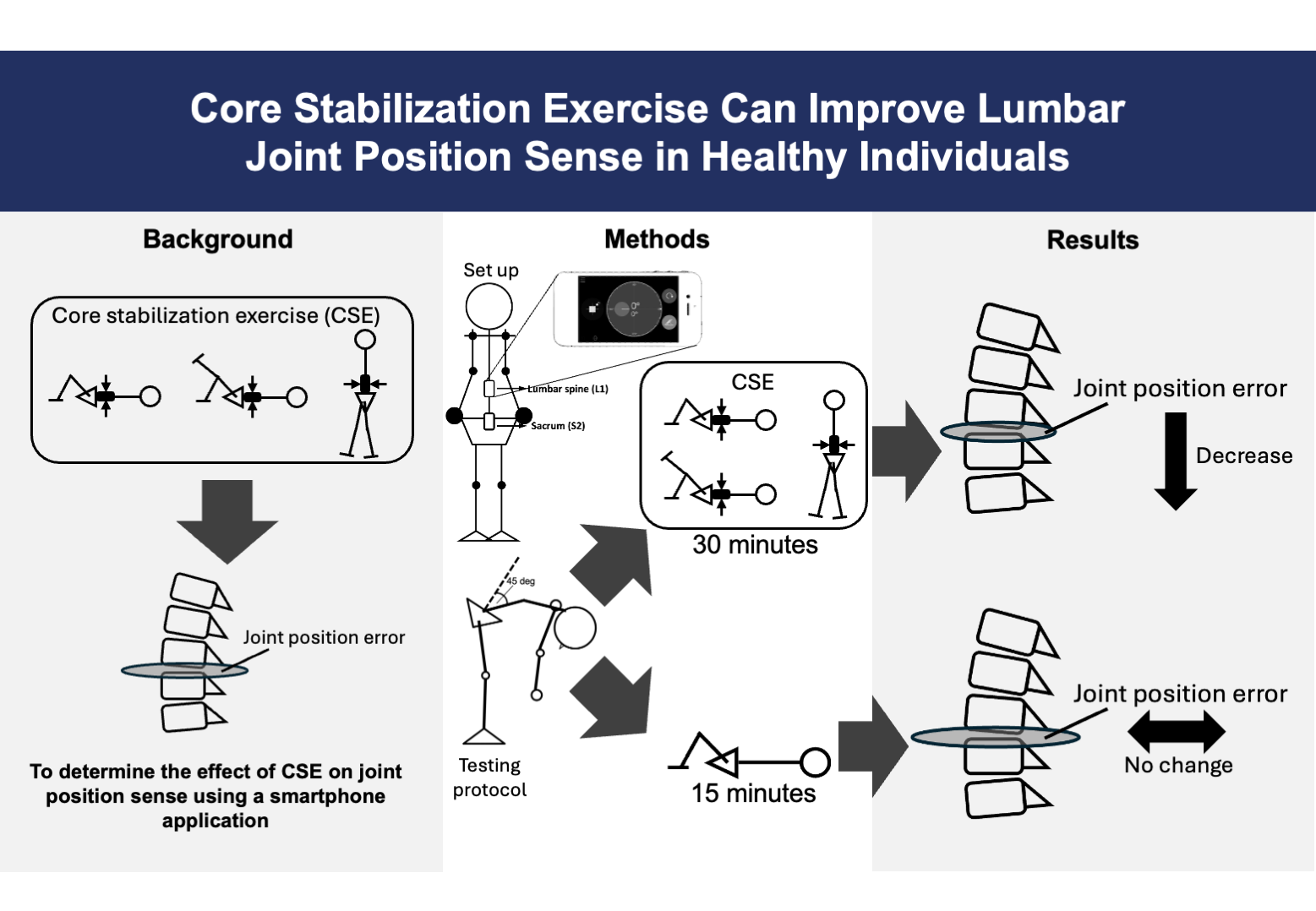
Background: Core stabilization exercises (CSE) are based on motor learning concepts focusing on sensorimotor function. It has been proposed that CSE can improve core stabilizer muscle function, leading to enhanced joint position sense. However, evidence to support the effects of CSE on joint position sense is still limited.
Objective: To compare the immediate effect of CSE on joint position sense of the lumbar spine using a smartphone application in healthy individuals.
Materials and methods: Fifty-six healthy individuals (9 males and 47 females) were recruited in the study. Two smartphones with the application were attached to the lumbar spine (L1) and sacrum (S2). They were asked to perform 45-degree lumbar flexion and return to neutral position, while lumbar joint position errors were recorded in each direction. They were then randomly assigned to CSE and control groups. After the intervention, they were asked to perform 45-degree lumbar flexion and return to a neutral position.
Results: The CSE group demonstrated significant improvement (p<0.05) in lumbar joint position sense during the 45-degree flexion, whereas the control group did not show improvement. Both groups did not show significant improvement during the return to a neutral position.
Conclusion: Findings suggested that one session of the CSE can improve lumbar joint position sense, which could be due to the increased activities of muscle spindles and Golgi tendon organs. In addition, our findings support the clinical utility of this smartphone application in measuring lumbar joint position sense.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Biely SA, Silfies SP, Smith SS, Hicks GE. Clinical observation of standing trunk movements: What do the aberrant movement patterns tell us? J Orthop Sports Phys Ther. 2014; 44(4): 262-72. doi:10.2519/ jospt.2014.4988
Wattananon P, Ebaugh D, Biely SA, Smith SS, Hicks GE, Silfies SP. Kinematic characterization of clinically observed aberrant movement patterns in patients with non-specific low back pain: a cross-sectional study. BMC Musculoskelet Disord. 2017; 18(1): 455. doi:10.1186/s12891-017-1820-x
Spinelli BA, Wattananon P, Silfies S, Talaty M, Ebaugh D. Using kinematics and a dynamical systems approach to enhance understanding of clinically observed aberrant movement patterns. Man Ther. 2015/02/01/ 2015; 20(1): 221-6. doi.org/10.1016/j. math.2014.07.012
Borghuis J, Hof AL, Lemmink KA. The importance of sensory-motor control in providing core stability: Implications for measurement and training. Sports Med. 2008; 38(11): 893-916. doi:10.2165/00007256- 200838110-00002
Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol. 2003; 13(4): 371-9. doi: 10.1016/s1050-6411(03)00044-0.
Proske U, Gandevia SC. The proprioceptive senses: their roles in signaling body shape, body position and movement, and muscle force. Physiol Rev. 2012; 92(4): 1651-97. doi:10.1152/physrev.00048.2011
Renkawitz T, Boluki D, Grifka J. The association of low back pain, neuromuscular imbalance, and trunk extension strength in athletes. Spine J. 2006; 6(6): 673-83. doi:10.1016/j.spinee.2006.03.012
Knox MF, Chipchase LS, Schabrun SM, Romero RJ, Marshall PWM. Anticipatory and compensatory postural adjustments in people with low back pain: a systematic review and meta-analysis. Spine J. 2018; 18(10): 1934-49. doi:10.1016/j.spinee.2018.06.008
Bussey MD, Aldabe D, Shemmell J, Jowett T. Anticipatory postural control differs between low back pain and pelvic girdle pain patients in the absence of visual feedback. Hum Mov Sci. 2020; 69: 102529. doi:10.1016/j.humov.2019.102529
Hodges PW, Barbe MF, Loggia ML, Nijs J, Stone LS. Diverse role of biological plasticity in low back pain and its impact on sensorimotor control of the spine. J Orthop Sports Phys Ther. 2019; 49(6): 389-401. doi:10.2519/jospt.2019.8716
Brumagne S, Diers M, Danneels L, Moseley GL, Hodges PW. Neuroplasticity of sensorimotor control in low back pain. J Orthop Sports Phys Ther. 2019; 49(6): 402-14. doi:10.2519/jospt.2019.8489
Selkow NM, Eck MR, Rivas S. Transversus abdominis activation and timing improves following core stability training: a randomized trial. Int J Sports Phys Ther. 2017; 12(7): 1048-56. doi:10.26603/ijspt20171048
Akuthota V, Ferreiro A, Moore T, Fredericson M. Core stability exercise principles. Curr Sports Med Rep. 2008; 7(1): 39-44. doi:10.1097/01.Csmr.0000 308663.13278.69
Hlaing SS, Puntumetakul R, Khine EE, Boucaut R. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord. 2021; 22(1): 998. doi:10.1186/s12891-021-04858-6
Kim TH, Kim E-H, Cho H-y. The effects of the CORE programme on pain at rest, movement-induced and secondary pain, active range of motion, and proprioception in female office workers with chronic low back pain: a randomized controlled trial. Clin Rehabil. 2014; 29(7): 653-62. doi:10.1177/0269215 514552075
Boucher J-A, Preuss R, Henry SM, Dumas J-P, Larivière C. The effects of an 8-week stabilization exercise program on lumbar movement sense in patients with low back pain. BMC Musculoskelet Disord. 2016; 17(1): 23. doi:10.1186/s12891-016- 0875-4
Puntumetakul R, Chalermsan R, Hlaing SS, Tapanya W, Saiklang P, Boucaut R. The effect of core stabilization exercise on lumbar joint position sense in patients with subacute non-specific low back pain: a randomized controlled trial. J Phys Ther Sci. 2018; 30(11): 1390-5. doi:10.1589/jpts.30.1390
Caña-Pino A, Espejo-Antúnez L, Adsuar JC, ApoloArenas MD. Test-retest reliability of an iPhone® inclinometer application to assess the lumbar joint repositioning error in non-specific chronic low back pain. Int J Environ Res Public Health. 2021; 18(5): 2489. doi:10.3390/ijerph18052489
Edwards SE, Lin YL, King JH, Karduna AH. Joint position sense - There׳s an app for that. J Biomech. 2016; 49(14): 3529-33. doi:10.1016/j.jbiomech.2016.07.033
Fox JA, Luther L, Epner E, LeClere L. Shoulder proprioception: A review. J Clin Med. 2024; 13(7): 2077. doi:10.3390/jcm13072077
Ravi B, Kapoor M, Player D. Feasibility and reliability of a web-based smartphone application for joint position measurement. J Rehabil Med. 2021; 53(5): jrm00188. doi:10.2340/16501977-2780
Wattananon P, Klomjai W, Sung W. One session of motor control exercise improves joint position sense assessed by an iPhone application: a randomized controlled trial. J Phys Ther Sci. 2019; 31(7): 583-9. doi:10.1589/jpts.31.583
Pope MH. Biomechanics of the lumbar spine. Ann Med. 1989; 21(5): 347-51. doi:10.3109/0785389890 9149219
Laird RA, Gilbert J, Kent P, Keating JL. Comparing lumbo-pelvic kinematics in people with and without back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014; 15: 229. doi:10. 1186/1471-2474-15-229
Tong MH, Mousavi SJ, Kiers H, Ferreira P, Refshauge K, van Dieën J. Is there a relationship between lumbar proprioception and low back pain? A systematic review with meta-analysis. Arch Phys Med Rehabil. 2017; 98(1): 120-36.e2. doi:10.1016/j. apmr.2016.05.016
Koumantakis GA, Winstanley J, Oldham JA. Thoracolumbar proprioception in individuals with and without low back pain: intratester reliability, clinical applicability, and validity. J Orthop Sports Phys Ther. 2002; 32(7): 327-35. doi:10.2519/jospt. 2002.32.7.327 [
Newcomer K, Laskowski ER, Yu B, Larson DR, An KN. Repositioning error in low back pain. Comparing trunk repositioning error in subjects with chronic low back pain and control subjects. Spine (Phila Pa 1976). 2000; 25(2): 245-50. doi:10.1097/00007632- 200001150-00017