Swallowing problems and oral health status among dwelling older adults in the community
Main Article Content
Abstract
Background: Oral health factors affecting oral food processing may comprise swallowing. Swallowing problems are commonly observed in older adults and are associated with various complications such as malnutrition, dehydration, and an increased risk of aspiration pneumonia. Age-related physiological changes in the swallowing mechanism, along with chronic diseases and dry mouth, further elevate the risk of dysphagia in this population.
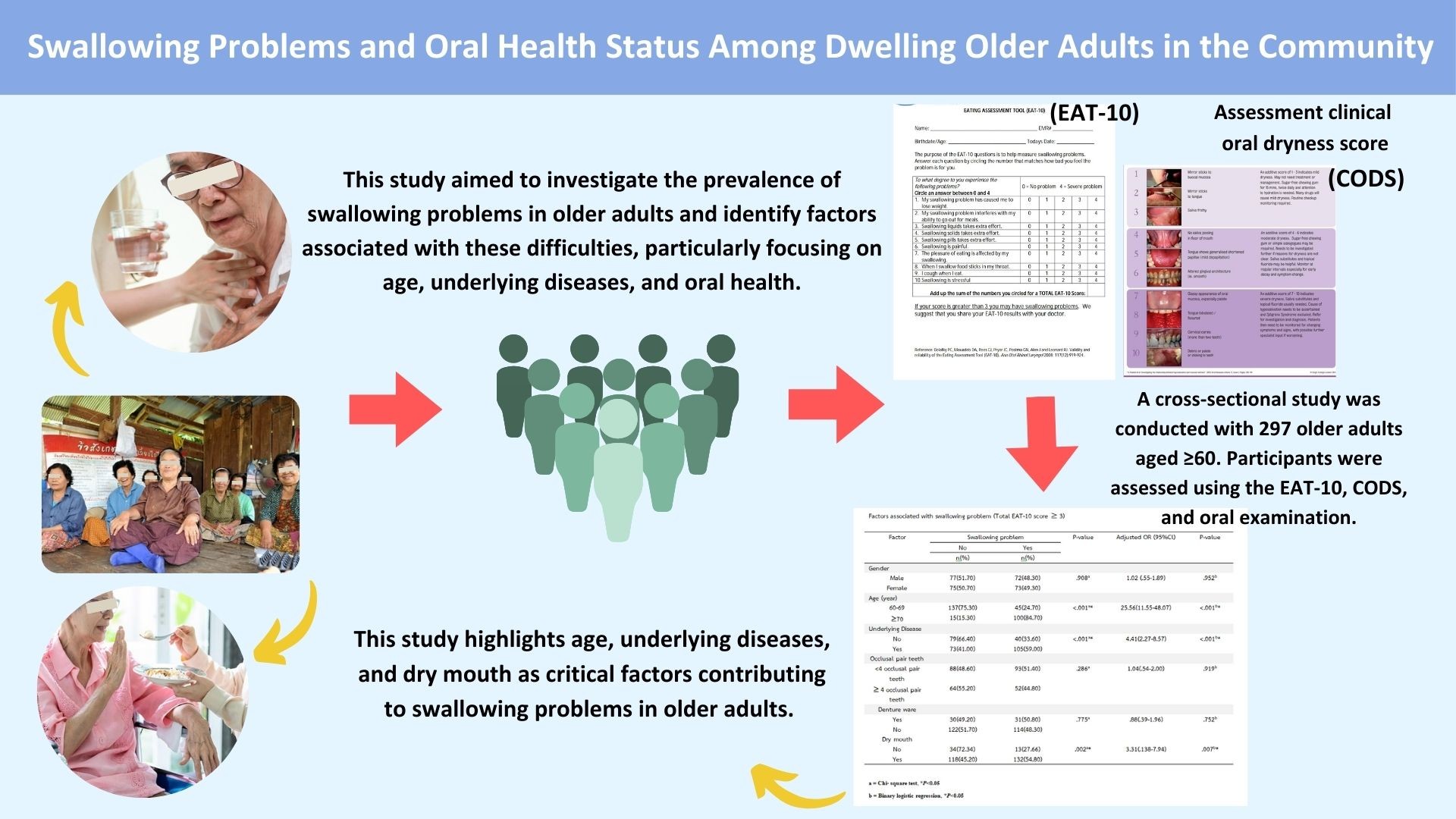
Objective: This study aimed to investigate the relationships between oral health status and swallowing problems in community-dwelling older adults from Sukhothai Province, Thailand.
Materials and methods: A cross-sectional study was conducted with 297 older adults aged 60 years and above, and a community-based study was conducted among the residents of Sukhothai province. Participants were assessed using the 10-item Eating Assessment Tool (EAT-10) questionnaire to evaluate swallowing problems. In addition, demographic data, underlying diseases, oral health status, and the incidence of dry mouth were recorded. The Thai Mental Status Examination (TMSE) was used to screen for cognitive function. Logistic regression analysis examined the association between these factors and the swallowing problem.
Results: The prevalence of swallowing problems was 48.8%. Swallowing problems were reported significantly with age, particularly in those aged ≥70 years, with a higher prevalence of swallowing issues at 84.7%, compared to 24.7% in participants aged 60-69 years (OR=25.56, p<0.001). Dry mouth was also strongly associated with swallowing problems. Participants suffering from dry mouth had higher odds of experiencing swallowing issues (OR=3.31, p><0.01). Underlying diseases further increased the risk of dysphagia (OR=4.41, p><0.001). No significant association was found between swallowing problems and gender, occlusal pairs, or denture use.><0.001). Dry mouth was also strongly associated with swallowing problems. Participants suffering from dry mouth had higher odds of experiencing swallowing issues (OR=3.31, p<0.01). Underlying diseases further increased the risk of dysphagia (OR=4.41, p<0.001). No significant association was found between swallowing problems and gender, occlusal pairs, or denture use.
Conclusion: 48.8% of community-dwelling older adults suffer from swallowing problems. This study highlights age, underlying diseases, and dry mouth as critical factors contributing to swallowing problems in older adults. Screening for swallowing issues in those aged ≥70 years, underlying disease, or dry mouth should be integrated into routine health assessments.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
United Nations Department of Economic and Social Affairs (UN DESA). World Population Prospects 2022. New York: United Nations; 2023.
National Economic and Social Development Council (NESDC). Thailand’s Population Projections 2010- 2040. Bangkok: National Economic and Social Development Board; 2021.
Sammasut R. Elderly Healthcare Management. Bangkok: Office of Elderly Affairs; 2009.
Baijens LW, Clave P, Cras P, Ekberg O, Forster A, Kolb GF, et al. European Society for Swallowing Disorders -European Union Geriatric Medicine Society White Paper: Oropharyngeal Dysphagia as a Geriatric Syndrome. Clin Interv Aging. 2016; 11: 1403-28. doi. org/10.2147/CIA.S107750.
Forster A, Samaras N, Gold G, Samaras D. Oropharyngeal dysphagia in older adults: a review. Eur Geriatr Med. 2011; 2(6): 356-362. doi:10.1016/j.eurger.2011.08.007.
Morley JE. Dysphagia and aspiration. J Am Med Dir Assoc. 2015; 16(8): 631-634. doi:10.1016/j.jamda.2015. 05.022.
Bastos RS, Lauris JRP, Bastos JRM, Velasco SRM, FogerTeixera D, Sa LM. The impacts of oral health-related quality of life of elderly people living at home: a crosssectional study. Cienc Saude Coletiva. 2021; 26: 1899- 1910. doi:10.1590/1413-81232021265.11962019.
Sheiham A, Steele JG, Marcenes W, Finch S, Walls AW. The impact of oral health on stated ability to eat certain foods; findings from the National Diet and Nutrition Survey of Older People in Great Britain. Gerodontology. 1999 Jul; 16(1): 11-20. doi:10.1111/ j.1741-2358.1999.00011.x.
Schindler JS, Kelly JH. Swallowing disorders in the elderly. The Laryngoscope. 2002 Apr;112(4):589- 602. doi:10.1097/00005537-200204000-00001.
Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012; 7: 287-98. doi:10.2147/cia.S23404.
Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008; 117(12): 919-24. doi: 10.1177/000348940811701210.
Korwanich K, Korwanich N, Kongma P, Klibngern H, Tavisak N. Validation of the Thai version of the Eating Assessment Tool-10 (Thai EAT-10). Chiang Mai: Faculty of Dentistry, Chiang Mai University; 2021.
Ueno M, Yanagisawa T, Shinada K, Ohara S, Kawaguchi Y. Masticatory ability and functional tooth units in Japanese adults. J Oral Rehabil. 2008; 35(5): 337-44. doi: 10.1111/j.1365-2842.2008.01847.x.
Osailan SM, Pramanik R, Shirlaw P, Proctor GB, Challacombe SJ. Clinical assessment of oral dryness: development of a scoring system related to salivary flow and mucosal wetness. J Oral Rehabil. 2012; 39(3): 185-94. doi:10.1111/j.1365-2842.2011.02253.x.
Chaleekrua S, Janpol K, Wattanapan P. Swallowing Problems among Community-Dwelling Elderly in Northeastern Thailand. J Prim Care Community Health. 2021; 12: 1-5. doi.org/10.1177/215013272110195.
Malandraki G, Robbins J. Dysphagia. Handb Clin Neurol. 2013;110:255-271. doi:10.1016/B978-0- 444-52901-5.00021-6.
Leira J, Maseda A, Lorenzo-Lopez L, Cibeira N, LopezLopez R, Lodeiro L, Millan-Calenti JC. Dysphagia and its association with other health-related risk factors in institutionalized older people: A systematic review. Arch Gerontol Geriatr. 2023; 110: 104991. doi:10.1016/j.archger.2023.104991.
Furuta M, Komiya-Nonaka M, Akifusa S, Shimazaki Y, Adachi M, Kinoshita T, et al. Interrelationship of oral health status, swallowing function, nutritional status, and cognitive ability with activities of daily living in Japanese elderly people receiving home care services due to physical disabilities. Community Dent Oral Epidemiol. 2013; 41(2): 173-81. doi:10.1111/ cdoe.12001.
Herrmann G, Muller K, Behr M, Hahnel S. Xerostomia and its impact on oral health-related quality of life. Z Gerontol Geriatr. 2017; 50: 145-50. doi:10.1007/ s00391-015-0968-y.
Furuya J. Effects of wearing complete dentures on swallowing in the elderly. Kokubyo Gakkai Zasshi. 1999; 66(4): 361-9. doi:10.5357/koubyou.66.361.
Ship JA, Pillemer SR, Baum BJ. Xerostomia and the geriatric patient. J Am Geriatr Soc. 2006; 50(3): 535- 43. doi.org/10.1046/j.1532-5415.2002.50123.x.
Celebic A, Knezovic-Zlataric D, Papic M, Carek V, Baucic I, Stipetic J. Factors related to patient satisfaction with complete denture therapy. J Gerontol A Biol Sci Med Sci. 2003; 58(10): M948-53. doi:10.1093/ gerona/58.10.M948.
Gil-Montoya JA, de Mello ALF, Barrios R, GonzalezMoles MA, Bravo M. Oral health in the elderly patient and its impact on general well-being: a nonsystematic review. Clin Interv Aging. 2015; 10: 461-7. doi.org/10.2147/CIA.S54630.
Sreebny LM, Schwartz SS. A reference guide to drugs and dry mouth-2nd Ed. Gerodontology. 2018; 35(1): 3-21. doi.org/10.1111/j.1741-2358.1997.00033.x.
Turner MD, Ship JA. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc. 2007; 138(suppl): 15S-20S. doi.org/10.14219/jada. archive.2007.0358.