Variation of sputum expectoration within day in bronchiectasis: Preliminary observational descriptive study
Main Article Content
Abstract
Background: Effective prescription of physical therapy airway clearance (ACT) is crucial for bronchiectasis patients, yet the optimal timing and frequency remain undefined. Understanding sputum expectoration patterns may determine the most suitable times for patients to undergo ACT.
Objective: This study aimed to investigate the daily sputum expectoration patterns in patients with bronchiectasis.
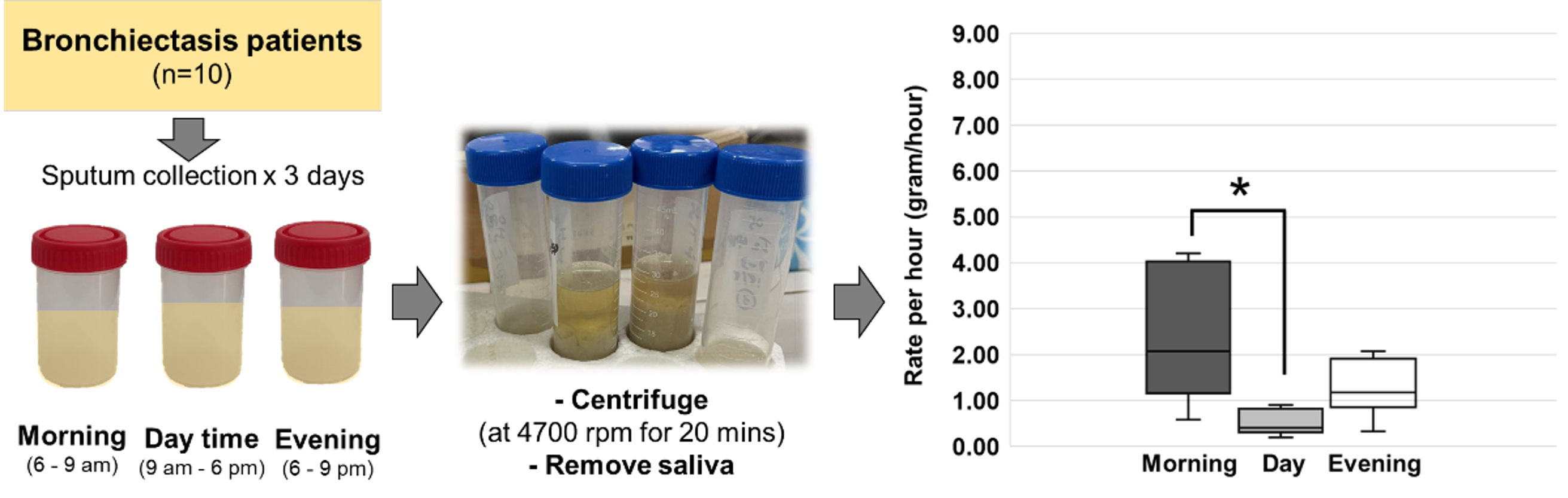
Materials and methods: Sputum was collected from ten bronchiectasis patients at home over three days, during morning (6 to 9 am), daytime (9 am to 6 pm), and evening (6 to 9 pm) periods. Collected sputum was centrifuged to remove saliva, weighed, and then converted to grams per hour for analysis.
Results: A total of 90 sputum containers were collected over three days from 10 patients. Most patients (N=8) expectorated a median (IQR) of 14.34 (7.96, 23.67) gm, showing a higher trend in the morning (2.07 (1.16, 4.03) gm/hr), followed by evening (1.18 (1.86, 1.92) g/hr) with the least during daytime (0.41 (0.32, 0.82) gm/hr). A minority of patients (N=2) with massive sputum production (72 and 63.98 for participant 1 and participant 2 respectively) exhibited the highest rate of expectoration during daytime (5.71 /hr), followed by the evening (3.83 /hr) and morning (1.69 /hr) on average over three days.
Conclusion: Most bronchiectasis patients exhibited higher rates of sputum expectoration in the morning and evening. Therefore, it is recommended to administer physical therapy for airway clearance twice daily, in the morning and evening, to prevent accumulation and enhance clearance.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Barker AF. Bronchiectasis. N Engl J Med. 2002; 346(18): 1383-93. doi: 10.1056/NEJMra012519.
Chalmers JD, Chang AB, Chotirmall SH, Dhar R, McShane PJ. Bronchiectasis. Nat Rev Dis Primers. 2018; 4(1): 45. doi: 10.1038/s41572-018-0042-3.
King PT. The pathophysiology of bronchiectasis. Int J Chron Obstruct Pulmon Dis. 2009; 4: 411-9. doi: 10.2147/copd.s6133.
Diego AD, Milara J, Martinez-Moragón E, Palop M, León M, Cortijo J. Effects of long-term azithromycin therapy on airway oxidative stress markers in noncystic fibrosis bronchiectasis. Respirol. 2013; 18(7): 1056-62. doi: 10.1111/resp.12130.
Olveira G, Olveira C, Dorado A, García-Fuentes E, Rubio E, Tinahones F, et al. Cellular and plasma oxidative stress biomarkers are raised in adults with bronchiectasis. Clin Nutr. 2013; 32(1): 112-7. doi:10.1016/j.clnu.2012.06.002.
King P, Daviskas E. Pathogenesis and diagnosis of bronchiectasis. Breathe. 2010; 6(4): 342-51. doi: 10. 1183/18106838.0604.342.
Semwal S, Mitra S, Singh SB. Autogenic drainage versus acapella for airway clearance in patients with bronchiectasis: randomized crossover trial. Int J Health Sci. 2015; (9): 5.
de Souza Simoni LH, dos Santos DO, de Souza HCD, Baddini-Martinez JA, Santos MK, Gastaldi AC. Acute effects of oscillatory pep and thoracic compression on secretion removal and impedance of the respiratory system in non–cystic fibrosis bronchiectasis. Respir Care. 2019; 64(7): 818-27. doi: 10.4187/respcare.06025.
Thompson CS. Randomised crossover study of the flutter device and the active cycle of breathing
technique in non-cystic fibrosis bronchiectasis. Thorax. 2002; 57(5): 446-8. doi: 10.1136/thorax.57.5.446.
Valente AM, Gastaldi AC, Cravo SL, Afonso JL, Sologuren MJJ, Guimarães RC. The effect of two techniques on the characteristics and transport of sputum in patients with bronchiectasis. Physiotherapy. 2004; 90(3): 158-64. doi: 10.1016/j.physio.2004.03.005.
Borsboom GJ, van Pelt W, van Houwelingen HC, van Vianen BG, Schouten JP, Quanjer PH. Diurnal variation in lung function in subgroups from two Dutch populations. Am J Respir Crit Care Med. 1999; 159(4): 1163-71. doi: 10.1164/ajrccm.159.4.9703106.
Button BM, Button B. Structure and function of the mucus clearance system of the lung. Cold Spring Harb Perspect Med. 2013; 3(8): a009720-a009720. doi: 10.1101/cshperspect.a009720.
Button B, Boucher RC. Role of mechanical stress in regulating airway surface hydration and mucus clearance rates. Respir Physiol Neurobiol. 2008; 163(1-3): 189-201. doi: 10.1016/j.resp.2008.04.020.
Bateman JR, Pavia D, Clarke SW. The retention of lung secretions during the night in normal subjects. Clin Sci Mol Med Suppl. 1978; 55(6): 523-7. doi: 10.1042/ cs0550523.
Braghiroli A, Braido F, Piraino A, Rogliani P, Santus P, Scichilone N. Day and night control of COPD and role of pharmacotherapy: a review. Int J Chron Obstruct Pulmon Dis. 2020; 15: 1269-85. doi: 10.2147/COPD. S240033.
Newton K, Malik V, Lee-Chiong T. Sleep and breathing. Clin Chest Med. 2014; 35(3): 451-6. doi: 10.1016/j. ccm.2014.06.001.
Hanning CD. Sleep and breathing ‘to sleep, perchance to breathe’ (with apologies to the bard). Intensive Crit Care Nurs. 1986; 2(1): 8-15. doi: 10.1016/0266- 612X(86)90069-6.
Kummer W, Lips KS, Pfeil U. The epithelial cholinergic system of the airways. Histochem Cell Biol. 2008; 130(2): 219-34. doi: 10.1007/s00418-008-0455-2.
Gaspar PM. Comparison of four standards for determining adequate water intake of nursing home residents. Res Theory Nurs Pract. 2011; 25(1): 11-22. doi: 10.1891/0889-7182.25.1.11
Rogers DF. Physiology of airway mucus secretion and pathophysiology of hypersecretion. Respir Care. 2007; 52(9): 1134-46.
Dwyer TJ, Zainuldin R, Daviskas E, Bye PTP, Alison JA. Effects of treadmill exercise versus Flutter® on respiratory flow and sputum properties in adults with cystic fibrosis: a randomised, controlled, cross-over trial. BMC Pulm Med. 2017; 17(1): 14. doi: 10.1186/ s12890-016-0360-8.
Lannefors L, Wollmer P. Mucus clearance with three chest physiotherapy regimes in cystic fibrosis: a comparison between postural drainage, PEP and physical exercise. Eur Resplr J. 1992; 5: 748-53. doi: 10.1183/09031936.93.05060748
Wolff RK, Dolovich MB, Obminski G, Newhouse MT. Effects of exercise and eucapnic hyperventilation on bronchial clearance in man. J Appl Physiol. 1977; 43(1): 46-50. doi: 10.1152/jappl.1977.43.1.46.
King PT, Holdsworth SR, Freezer NJ, Villanueva E, Holmes PW. Characterisation of the onset and presenting clinical features of adult bronchiectasis. Respir Med. 2006; 100(12): 2183-9. doi: 10.1016/j. rmed.2006.03.012.
Costa JC, Machado JN, Ferreira C, Gama J, Rodrigues C. The bronchiectasis severity index and FACED score for assessment of the severity of bronchiectasis. Pulmonology. 2018; 24(3): 149-54. doi: 10.1016/j. rppnen.2017.08.009.