Phrenic nerve and cervical functional interdependence and its sensorimotor anomalies: A musculoskeletal pain consideration review
Main Article Content
Abstract
Background: Optimal breathing occurs when using the diaphragm muscle, which is known as diaphragmatic breathing. Any disruption or faulty habit of this breathing pattern would result in breathing pattern disorders (BPDs).
Objectives: The aim of this review is to shed light on the importance of detecting the presence and extent of asymptomatic functional anomalies of cervical segments among individuals with breathing pattern disorders.
Materials and methods: This narrative review was performed by searching in MEDLINE using terms related to phrenic nerve and cervical functional, interdependence, and sensorimotor anomalies. Additionally, articles regarding this topic were extracted in full for a comprehensive and critical analysis. Any study design, such as observational studies, systematic reviews, or narrative reviews, was included. The results were narratively synthesized and described.
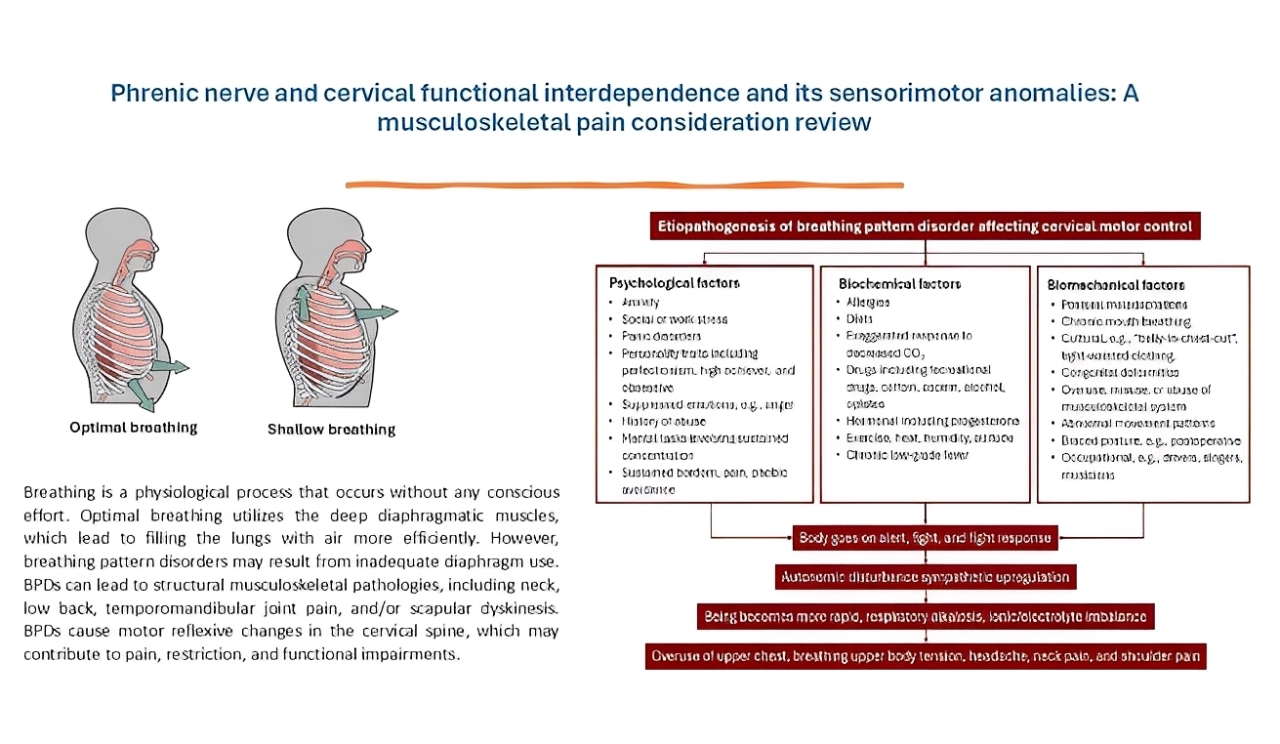
Results: Breathing is a physiological process that occurs without any conscious effort. Optimal breathing utilizes the deep diaphragmatic muscles, which lead to filling the lungs with air more efficiently. However, breathing pattern disorders may result from inadequate diaphragm use. BPDs can lead to structural musculoskeletal pathologies, including neck, low back, temporomandibular joint pain, and/or scapular dyskinesis. BPDs cause motor reflexive changes in the cervical spine, which may contribute to pain, restriction, and functional impairments.
Conclusion: Early identification of this faulty habitual suboptimal breathing is required to minimize its adverse effect, which can be disruptive to the motor control mechanism.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Pryor JA, Prasad SA, editors. Physiotherapy for respiratory and cardiac problems—adults and paediatrics. Edinburgh: Churchill Livingstone; 2002.
Kaminoff L. What yoga therapists should know about the anatomy of breathing. Int J Yoga Ther. 2006; 16: 67-77. doi:10.17761/ijyt.16.1.64603tq46513j242.
CliftonSmith T, Rowley J. Breathing pattern disorders and physiotherapy: inspiration for our profession. Phys Ther Rev. 2011; 16(1): 75-86. doi:10.1179/1743288X10Y.0000000025.
Chaitow L. Breathing pattern disorders, motor control, and low back pain. J Osteopath Med. 2004; 7(1): 33-40. doi:10.1016/S1443-8461(04)80007-8.
Courtney R, Cohen M, van Dixhoorn J. Relationship between dysfunctional breathing patterns and ability to achieve target heart rate variability with features of “coherence” during biofeedback. Altern Ther Health Med. 2011; 17: 38-44.
Perri M, Halford E. Pain and faulty breathing: a pilot study. J Bodyw Mov Ther. 2004; 8(4): 297-306. doi:10.1016/S1360-8592(03)00085-8.
Vickery R. The effect of breathing pattern retraining on performance in competitive cyclists [Internet]. 2008 [cited 2021 Mar 7]. Available from: /paper/The-effect-of-breathing-pattern-retraining-on-in-Vickery/80d5467cb0fb59f8e9777c943a8688ea6ecd8135.
Chaitow L, Gilbert C, Bradley D. Recognizing and treating breathing disorders. 2nd Ed. [Internet]. Elsevier; [cited 2021 Mar 2]. Available from: https://www.elsevier.com/books/recognizing-and-treating-breathing-disorders/chaitow/978-0-7020-4980-4.
Perri M. Rehabilitation of breathing pattern disorders. In: Liebenson C, editor. Rehabilitation of the spine: A practitioner’s manual. 2nd Ed. Philadelphia: Lippincott Williams and Wilkins; 2007: pp 93-109. J Can Chiropr Assoc. 2007; 51(1): 62.
Hodges PW, Heijnen I, Gandevia SC. Postural activity of the diaphragm is reduced in humans when respiratory demand increases. J Physiol. 2001; 537(Pt 3): 999-1008. doi:10.1111/j.1469-7793.2001.00999.
Kapreli E, Vourazanis E, Billis E, Oldham JA, Strimpakos N. Respiratory dysfunction in chronic neck pain patients. A pilot study. Cephalalgia. 2009; 29(7): 701-10. doi:10.1111/j.1468-2982.2008.01787.
Roussel NA, Nijs J, Truijen S, Smeuninx L, Stassijns G. Low back pain: clinimetric properties of the Trendelenburg test, active straight leg raise test, and breathing pattern during active straight leg raising. J Manipulative Physiol Ther. 2007; 30(4): 270-8. doi:10.1016/j.jmpt.2007.03.001.
Hruska RJ. Influences of dysfunctional respiratory mechanics on orofacial pain. Dent Clin North Am. 1997; 41(2): 211-27.
Courtney R. The functions of breathing and its dysfunctions and their relationship to breathing therapy. Int J Osteopath Med. 2009; 12(3): 78-85. doi: 10.1016/j.ijosm.2009.04.002.
Kolar P, Sulc J, Kyncl M, et al. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012; 42(4): 352-62. doi:10.2519/jospt.2012.3830.
Keleman S. Emotional anatomy: the structure of experience. Berkeley: Center Press; 1985.
Yu X, Jiang HY, Zhang CX, Jin ZH, Gao L, Wang RD, et al. The role of the diaphragm in postural stability and visceral function in Parkinson’s disease. Front Aging Neurosci. 2021; 13: 785020. doi:10.3389/fnagi.2021.785020.
Salah HM, Goldberg LR, Molinger J, Felker GM, Applefeld W, Rassaf T, et al. Diaphragmatic function in cardiovascular disease: JACC Review Topic of the Week. J Am Coll Cardiol. 2022; 80(17): 1647-59. doi:10.1016/j.jacc.2022.08.760.
Rice RL. Symptom patterns of the hyperventilation syndrome. Am J Med. 1950; 8(6): 691-700. doi:10.1016/0002-9343(50)90093-3.
Thomas M, McKinley RK, Freeman E, Foy C, Price D. The prevalence of dysfunctional breathing in adults in the community with and without asthma. Prim Care Respir J. 2005; 14(2): 78-82. doi:10.1016/j.pcrj.2004.10.007.
Lum LC. Hyperventilation syndromes in medicine and psychiatry: a review. J R Soc Med. 1987; 80(4): 229-31. doi:10.1177/014107688708000413.
Chapman EB, Hansen-Honeycutt J, Nasypany A, Baker RT, May J. A clinical guide to the assessment and treatment of breathing pattern disorders in the physically active: Part 1. Int J Sports Phys Ther. 2016; 11(5): 803-9.
Lucas KR, Polus BI, Rich PA. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. J Bodyw Mov Ther. 2004; 8(3): 160-6. doi: 10.1016/j.jbmt.2003.12.002.
Chapman EB, Hansen Honeycutt J, Nasypany A, Baker RT, May J. A clinical guide to the assessment and treatment of breathing pattern disorders in the physically active: part 1, a case series. Int J Sports Phys Ther. 2016; 11(6): 971-9.
Kapreli E, Vourazanis E, Billis E, Oldham JA, Strimpakos N. Respiratory dysfunction in chronic neck pain patients. A pilot study. Cephalalgia. 2009;29(7):701–10. doi:10.1111/j.1468 2982.2008.01787.
Kolnes LJ. Embodying the body in anorexia nervosa--a physiotherapeutic approach. J Bodyw Mov Ther. 2012; 16(3): 281-8. doi:10.1016/j.jbmt.2011.12.005.
Bennett SE, Schenk RJ, Simmons ED. Active range of motion utilized in the cervical spine to perform daily functional tasks. J Spinal Disord Tech. 2002; 15(4): 307-11. doi:10.1097/00024720-200208000-00008.
Binder AI. Cervical spondylosis and neck pain. BMJ. 2007; 334(7592): 527-31. doi:10.1136/bmj.39130.530182.80.
Fejer R, Hartvigsen J. Neck pain and disability due to neck pain: what is the relation?. Eur Spine J. 2008; 17(1): 80-8. doi:10.1007/s00586-007-0521-9.
Abhishek A, Doherty M. Diagnosis and clinical presentation of osteoarthritis. Rheum Dis Clin North Am. 2013; 39(1): 45-66. doi:10.1016/j.rdc.2012.10.007.
Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual, Vol. 2, The Lower Extremities. 1st Ed. Baltimore: Williams & Wilkins; 1993; pp 628.
Bradley H, Esformes J. Breathing pattern disorders and functional movement. Int J Sports Phys Ther. 2014; 9(1): 28-39.
Barraclough A, Triplett J, Tuch P. Brachial neuritis with phrenic nerve involvement. J Clin Neurosci. 2012; 19(9): 1301-2. doi:10.1016/j.jocn.2011.12.009.
Prakash, Prabhu LV, Madhyastha S, Singh G. A variation of the phrenic nerve: case report and review. Singapore Med J. 2007; 48(12): 1156-7.
Messlinger K, Fischer MJ, Lennerz JK. Neuropeptide effects in the trigeminal system: pathophysiology and clinical relevance in migraine. Keio J Med. 2011; 60(3): 82-9. doi:10.2302/kjm.60.82.
Kemp WJ 3rd, Tubbs RS, Cohen-Gadol AA. The innervation of the cranial dura mater: neurosurgical case correlates and a review of the literature. World Neurosurg. 2012; 78(5): 505-10. doi:10.1016/j.wneu.2011.10.045.
Adeeb N, Mortazavi MM, Tubbs RS, Cohen-Gadol AA. The cranial dura mater: a review of its history, embryology, and anatomy. Childs Nerv Syst. 2012; 28(6): 827-37. doi:10.1007/s00381-012-1744-6.
Upadhyay J, Knudsen J, Anderson J, Becerra L, Borsook D. Noninvasive mapping of human trigeminal brainstem pathways. Magn Reson Med. 2008; 60(5): 1037-46. doi:10.1002/mrm.21682.
Kahkeshani K, Ward PJ. Connection between the spinal dura mater and suboccipital musculature: evidence for the myodural bridge and a route for its dissection--a review. Clin Anat. 2012; 25(4): 415-22. doi:10.1002/ca.21261.
Dean NA, Mitchell BS. Anatomic relation between the nuchal ligament (ligamentum nuchae) and the spinal dura mater in the craniocervical region. Clin Anat. 2002; 15(3): 182-5. doi:10.1002/ca.10001.
Cavanaugh JM, Lu Y, Chen C, Kallakuri S. Pain generation in lumbar and cervical facet joints. J Bone Joint Surg Am. 2006; 88(Suppl2): 63-7. doi:10.2106/JBJS.E.01411.
Abrahams VC. The physiology of neck muscles; their role in head movement and maintenance of posture. Can J Physiol Pharmacol. 1977; 55(3): 332-8. doi:10.1139/y77-047.
McLain RF. Mechanoreceptor endings in human cervical facet joints. Spine (Phila Pa 1976). 1994; 19(5): 495-501. doi: 10.1097/00007632-199403000-00001.
Kulkarni V, Chandy MJ, Babu KS. Quantitative study of muscle spindles in suboccipital muscles of human foetuses. Neurol India. 2001; 49(4): 355-9.
Proske U, Gandevia SC. The proprioceptive senses: their roles in signaling body shape, body position and movement, and muscle force. Physiol Rev. 2012; 92(4): 1651-97. doi:10.1152/physrev.00048.2011.
Grgić V. Cervicogenic headache: etiopathogenesis, characteristics, diagnosis, differential diagnosis and therapy. Lijec Vjesn. 2007; 129(6-7): 230-6.
Tropp H. Commentary: Functional ankle instability revisited. J Athl Train. 2002; 37(4): 512-5.
McPartland JM, Brodeur RR, Hallgren RC. Chronic neck pain, standing balance, and suboccipital muscle atrophy—a pilot study. J Manipulative Physiol Ther. 1997; 20(1): 24-9.
Madeleine P, Prietzel H, Svarrer H, Arendt Nielsen L. Quantitative posturography in altered sensory conditions: a way to assess balance instability in patients with chronic whiplash injury. Arch Phys Med Rehabil. 2004; 85(3): 432-8. doi:10.1016/j.apmr.2003.03.003.
Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992; 5(4): 383-97. doi:10.1097/00002517-199212000-00001.
Check JH, Cohen R, Katsoff B, Check D. Hypofunction of the sympathetic nervous system is an etiologic factor for a wide variety of chronic treatment-refractory pathologic disorders which all respond to therapy with sympathomimetic amines. Med Hypotheses. 2011; 77(5): 717-25. doi:10.1016/j.mehy.2011.08.024.
Cohen H, Neumann L, Shore M, Amir M, Cassuto Y, Buskila D. Autonomic dysfunction in patients with fibromyalgia: application of power spectral analysis of heart rate variability. Semin Arthritis Rheum. 2000; 29(4): 217-27. doi:10.1053/sarh.2000.3621.
Hallman DM, Lyskov E. Autonomic regulation, physical activity and perceived stress in subjects with musculoskeletal pain: 24-hour ambulatory monitoring. Int J Psychophysiol. 2012; 86(3): 276-82. doi:10.1016/j.ijpsycho.2012.09.004.
Fonseca D, Beda A, Sá A, Simpson D. Gain and coherence estimates between respiration and heart-rate: Differences between inspiration and expiration. Auton Neurosci. 2013; 178: doi:10.1016/j.autneu.2013.02.013.
Restrepo CS, Eraso A, Ocazionez D, Lemos J, Martinez S, Lemos DF. The diaphragmatic crura and retrocrural space: normal imaging appearance, variants, and pathologic conditions. Radiographics. 2008; 28(5): 1289-305. doi:10.1148/rg.285085022.
Gest TR, Hildebrandt S. The pattern of the thoracic splanchnic nerves as they pass through the diaphragm. Clin Anat. 2009; 22(7): 809-14. doi:10.1002/ca.20867.
Zou Y, Zhao X, Hou YY, Liu T, Wu Q, Huang YH, et al. Meta-analysis of effects of voluntary slow breathing exercises for control of heart rate and blood pressure in patients with cardiovascular diseases. Am J Cardiol. 2017; 120(1): 148-53. doi:10.1016/j.amjcard.2017.03.009.
Loukas M, Klaassen Z, Merbs W, Tubbs RS, Gielecki J, Zurada A. A review of the thoracic splanchnic nerves and celiac ganglia. Clin Anat. 2010; 23(5): 512-22. doi:10.1002/ca.21018.
Loukas M, Du Plessis M, Louis RG, Tubbs RS, Wartmann CT, Apaydin N. The subdiaphragmatic part of the phrenic nerve - morphometry and connections to autonomic ganglia. Clin Anat. 2016; 29(1): 120-8. doi:10.1002/ca.22577.
Iams J. When reflex rule: A new paradigm in understanding why some people don’t get well [Internet]. Primal Reflex Release Technique; [cited 2021 Mar 29]. Available from: https://theprrt.com/pain-relief-articles/.
Fantazzi F. Primal Reflex Release Technique Part 1 - PRRT Physical Therapy - CyberPT [Internet]. [cited 2021 Mar 22]. Available from: http://www.cyberpt.com/prrt.asp.
Javanshir K, Ortega-Santiago R, Mohseni-Bandpei MA, Miangolarra-Page JC, Fernández-de-Las-Peñas C. Exploration of somatosensory impairments in subjects with mechanical idiopathic neck pain: a preliminary study. J Manipulative Physiol Ther. 2010; 33(7): 493-9. doi:10.1016/j.jmpt.2010.07.005.
Wehrwein EA, Joyner MJ. Chapter 8 - Regulation of blood pressure by the arterial baroreflex and autonomic nervous system. In: Buijs RM, Swaab DF, Editors. Handbook of Clinical Neurology [Internet]. Elsevier; 2013 [cited 2025 Feb 16]. pp 89-102. (Autonomic Nervous System; vol. 117). Available from: https://www.sciencedirect.com/science/article/pii/B9780444534910000080.
Sueki DG, Cleland JA, Wainner RS. A regional interdependence model of musculoskeletal dysfunction: research, mechanisms, and clinical implications. J Man Manip Ther. 2013; 21(2): 90-102. doi:10.1179/2042618613Y.0000000059.
Myers TW. Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists. Elsevier Health Sciences; 2009: pp 308.