Radiation safety assessment of patient and staff during intracranial aneurysm treatment: A phantom study
Main Article Content
Abstract
Background: Endovascular treatment using coiling embolization for intracranial aneurysms is common in interventional neuroradiology (INR). However, it is associated with high radiation exposure to both patients and medical staff. The assessment and management of radiation risk have been a concern.
Objective: To evaluate patient and scatter radiation doses at INR staff working position during the coiling embolization procedure in a phantom study.
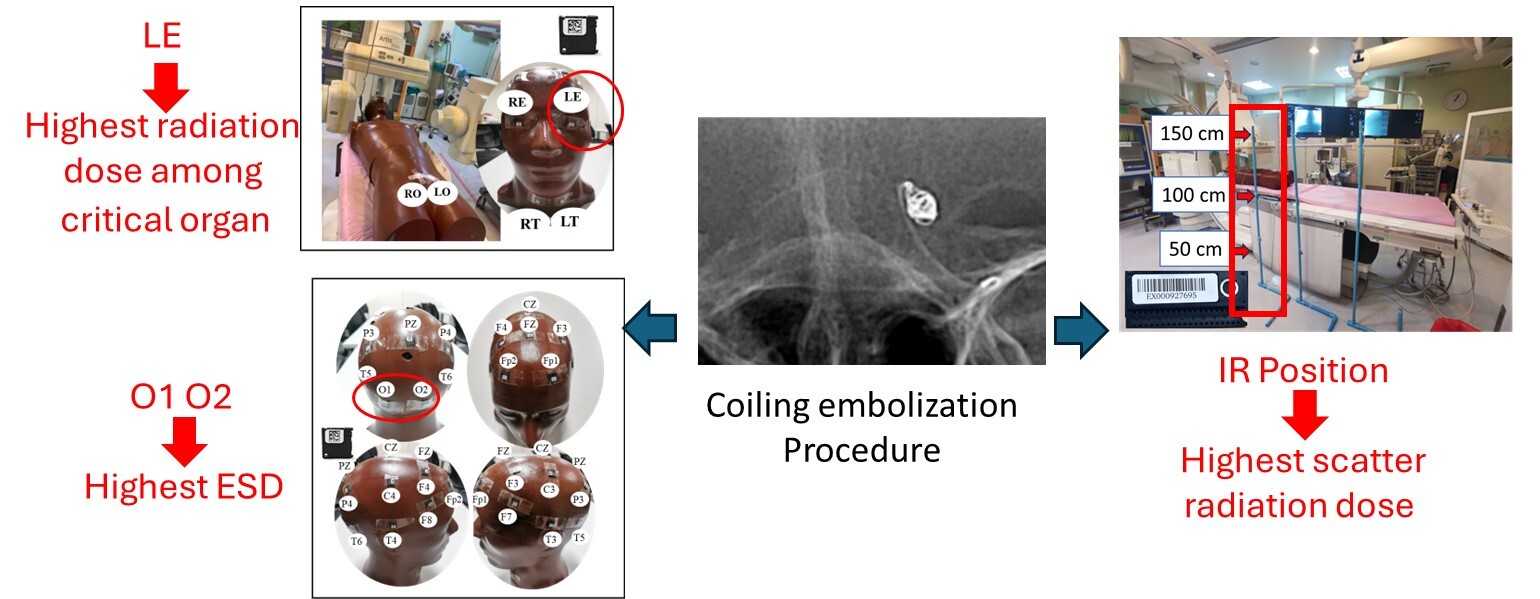
Materials and methods: An anthropometric phantom from head to pelvis was placed on an angiographic table. To determine the phantom’s entrance skin dose (ESD), 19 NanoDot optically stimulated luminescence dosimeters (OSLDs) were placed on the surface of the head phantom. Moreover, 6 NanoDot OSLDs were also placed on the surface of the phantom at 3 critical organs (eyes, thyroid, ovaries). To determine the scatter radiation dose at staff working position, polyvinyl chloride pipes (150 cm height) were placed at the position of all staff, including interventional radiologist (IR), radiology resident (RR), scrubbed nurse (SN), radiologic technologist (RT), circulating nurse (CN), and nurse anesthetists (AN). The InLight® OSLDs were placed on each PVC pipe at 50, 100, and 150 cm height from the floor level. Coiling embolization was simulated following the standard procedure using a bi-plane digital subtraction angiography unit with standard radiation protective equipment. The patient doses from the radiation dose structured report (RDSR) were also recorded.
Results: The highest ESDs were observed in the occipital part (1,631.56±36.97 mGy). These ESD peaks were also observed within the safety limit and produced no skin reaction. The radiation dose at the left eye was observed to be the highest value among critical organs. The highest scatter radiation dose was observed at the position of IR at 100 cm level. Among CN, AN, and RT positions, the highest dose was recorded at the RT position at the level of 150 cm. The RDSR showed that most of the patient radiation dose was received from the 2-dimension angiography.
Conclusion: The distribution of radiation dose varied across different staff positions. As the key person conducting the coiling embolization procedure, the IR position received the highest radiation dose. Thus, close monitoring and development of additional radiation protection methods for this position are essential. Although the radiation dose at the back of the head was elevated, it remained within safety limits. Nevertheless, the monitoring of potential radiation effects should not be neglected.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Molyneux AJ, Kerr RSC, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet Lond Engl. 2005; 366(9488): 809-17. doi: 10.1016/S0140 6736(05)67214-5.
Luo M, Yang S, Ding G, Xiao Q. Endovascular coiling versus surgical clipping for aneurysmal subarachnoid hemorrhage: A meta-analysis of randomized controlled trials. J Res Med Sci Off J Isfahan Univ Med Sci. 2019; 24: 88. doi: 10.4103/jrms.JRMS_414_18.
Zhu W, Ling X, Petersen JD, Liu J, Xiao A, Huang J. Clipping versus coiling for aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis of prospective studies. Neurosurg Rev. 2022; 45(2): 1291-302. doi: 10.1007/s10143-021-01704-0.
Hamada N, Fujimichi Y. Classification of radiation effects for dose limitation purposes: history, current situation and future prospects. J Radiat Res. 2014; 55(4): 629-40. doi: 10.1093/jrr/rru019.
Clement CH, Stewart FA, Akleyev AV, Hauer-Jensen M, Hendry JH, Kleiman NJ, et al. ICRP PUBLICATION 118: ICRP Statement on Tissue Reactions and Early and Late Effects of Radiation in Normal Tissues and Organs — Threshold Doses for Tissue Reactions in a Radiation Protection Context. Ann ICRP. 2012; 41(1 2): 1-322. doi: 10.1016/j.icrp.2012.02.001.
National Research Council (US) Committee on Health Effects of Exposure to Low Levels of Ionizing Radiations (BEIR VII). Health Effects of Exposure to Low Levels of Ionizing Radiations: Time for Reassessment? Washington (DC): National Academies Press (US); 1998. doi: 10.172 26/1224.
Chida K, Kato M, Kagaya Y, Zuguchi M, Saito H, Ishibashi T, et al. Radiation dose and radiation protection for patients and physicians during interventional procedure. J Radiat Res. 2010; 51(2): 97-105. doi: 10.1269/jrr.09112.
Kirisattayakul W, Pattum P, Munkong W, Prabsattroo T, Khottapat C, Chomkhunthod T, et al. Comparing Radiation Dose of Cerebral Angiography Using Conventional and High kV Techniques: A Retrospective Study on Intracranial Aneurysm Patients and a Phantom Study. Tomography. 2023; 9(2): 621-32. doi: 10.3390/ tomography9020050.
Riabroi K, Khanungwanitkul K, Wattanapongpitak P, Krisanachinda A, Hongsakul K. Patient Radiation Dose in Neurointerventional Radiologic Procedure: A Tertiary Care Experience. Neurointervention. 2018; 13(2): 110-6. doi: 10.5469/neuroint.2018.00983.
Sánchez RM, Vañó E, Fernández JM, Rosati S, López Ibor L. Radiation Doses in Patient Eye Lenses during Interventional Neuroradiology Procedures. AJNR Am J Neuroradiol. 2016; 37(3): 402-7. doi: 10.3174/ajnr. A4549.
Tamam N, Salah H, Almogren KS, Mahgoub O, Saeed MK, Abdullah Y, et al. Evaluation of patients’ and occupational radiation risk dose during conventional and interventional radiology procedures. Radiat Phys Chem. 2023; 207: 110818. doi: 10.1016/j.radphyschem. 2023.110818.
Wen CS, Lin SM, Chen Y, Chen JC, Wang YH, Tseng SH. Radiation-induced temporary alopecia after embolization of cerebral arteriovenous malformations. Clin Neurol Neurosurg. 2003; 105(3): 215-7. doi: 10.1016/s0303 8467(03)00007-6.
Ounsakul V, Iamsumang W, Suchonwanit P. Radiation- Induced Alopecia after Endovascular Embolization under Fluoroscopy. Case Rep Dermatol Med. 2016; 2016: 8202469. doi: 10.1155/2016/8202469.
Cammann VL, Schweiger V, Cieslik M, Seifert B, Gilhofer T, Koleva I, et al. Effectiveness of radiation protection systems in the cardiac catheterization laboratory: a comparative study. Clin Res Cardiol. 2023; 112(5): 605-13. doi: 10.1007/s00392-022-02142-8.
Jansen MM, Koster A, van Herwaarden JA, Hazenberg CEVB. Reduction of Occupational Radiation Exposure During Endovascular Treatment of Peripheral Artery Disease Using Radiation Absorbing Drapes. Ann Vasc Surg. 2022; 84: 336-43. doi: 10.1016/j.avsg.2022.01.030.
Vlastra W, Delewi R, Sjauw KD, Beijk MA, Claessen BE, Streekstra GJ, et al. Efficacy of the RADPAD Protection Drape in Reducing Operators’ Radiation Exposure in the Catheterization Laboratory: A Sham- Controlled Randomized Trial. Circ Cardiovasc Interv. 2017; 10(11): e006058. doi: 10.1161/CIRCINTER- VENTIONS. 117.006058.
Awikunprasert P, Somtom T, Somboot T, Kittichotwarat S, Damchoo P, Mongkolratnan A, et al. Radiation dose in radiologist from cerebral angiography using optically stimulated luminescence dosimeter. J Assoc Med Sci. 2023; 57: 29-37. doi: 10.12982/JAMS.2024.004.
Meijer EJ, van Zandvoort DWH, Loos MJA, Tseng CMESN, van Pul C. The eye lens dose of the interventionalist: Measurement in practice. Phys Med. 2022; 100: 1-5. Doi: doi.org/10.1016/j.ejmp.2022. 05.012.
Yamada A, Haga Y, Sota M, Abe M, Kaga Y, Inaba Y, et al. Eye Lens Radiation Dose to Nurses during CardiacInterventional Radiology: An Initial Study. Diagn Basel Switz. 2023; 13(18): 3003. doi: 10.3390/diagnostics 13183003.
Calvanese F, Auricchio AM, Pohjola A, Hafez A, Nurminen V, Korja M, et al. Changes in treatment of intracranial aneurysms during the last decade in a large European neurovascular center. Acta Neurochir (Wien). 2024; 166(1): 173. doi: 10.1007/s00701-024-06064-4.
Hayashi S, Takenaka M, Kogure H, Yakushijin T, Nakai Y, Ikezawa K, et al. A follow-up questionnaire survey 2022 on radiation protection among 464 medical staff from 34 endoscopy–fluoroscopy departments in Japan. DEN Open. 2023; 3(1): e227. doi: 10.1002/ deo2.227
Meijer EJ, van Zandvoort DWH, Loos MJA, Tseng CMESN, van Pul C. The eye lens dose of the interventionalist: Measurement in practice. Phys Med. 2022; 100: 1-5. doi: 10.1016/j.ejmp.2022.05.012.
Schauer DA, Linton OW. National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. Radiology. 2009; 253(2): 293-6. doi: 10.1148/radiol.2532090494.
Harrison JD, Balonov M, Bochud F, Martin CJ, Menzel HG, Smith-Bindman R, et al. The use of dose quantities in radiological protection: ICRP publication 147 Ann ICRP 50(1) 2021. J Radiol Prot Off J Soc Radiol Prot. 2021; 41(2). doi: 10.1088/1361-6498/abe548.
Schueler BA, Kallmes DF, Cloft HJ. 3D Cerebral Angiography: Radiation Dose Comparison with Digital Subtraction Angiography. Am J Neuroradiol. 2005; 26(8): 1898-901.
Andres C, Agulla M, Torres R, Perez-Garcia H, del Castillo A, Miguel D, et al. Patient doses in a biplane angiography system. Phys Med. 2016; 32: 307. doi: 10.1016/j.ejmp.2016.07.165.
Gkanatsios N, Huda W, Peters K. How does magnification affect image quality and patient dose in digital subtraction angiography? Proc SPIE. 2001; 4320: 326-30. doi: 10.1117/12.430927
Song Y, Kim Y, Han S, Kim TI, Choi JH, Maeng JY, et al. Estimated radiation dose according to the craniocaudal angle in cerebral digital subtraction angiography: Patient and phantom study. J Neuroradiol. 2019; 46(6): 345-50. doi: 10.1016/j.neurad.2019.07. 003.
Munkong W, Kirisattayakul W, Pattum P, Kianprasit J, Prabsattroo T, Punikhom P, et al. Analysis of patient radiation dose and angiographic techniques during intracranial aneurysmal diagnosis: a 5-year experience of interventional neuroradiology unit in Srinagarind Hospital. J Assoc Med Sci. 2021 ; 54(1): 67-75. doi: 10.14456/jams.2021.9.
Yi HJ, Sung JH, Lee DH, Kim SW, Lee SW. Analysis of Radiation Doses and Dose Reduction Strategies During Cerebral Digital Subtraction Angiography. World Neurosurg. 2017; 100: 216-23. doi: 10.1016/j. wneu.2017.01.004.
Mancosu P, Ripamonti D, Veronese I, Cantone MC, Giussani A, Tosi G. Angular dependence of the TL reading of thin alpha-Al2O3:C dosemeters exposed to different beta spectra. Radiat Prot Dosimetry. 2005; 113(4): 359-65. doi: 10.1093/rpd/nch476.
Okazaki T, Hayashi H, Takegami K, Okino H, Kimoto N, Maehata I, et al. Fundamental Study of nanoDot OSL Dosimeters for Entrance Skin Dose Measurement in Diagnostic X-ray Examinations. J Radiat Prot Res. 2016;41(3): 229-36. doi: 10.14407/jrpr.2016.41.3.229.
Vaccaro M, Guarneri F, Brianti P, Cannavò SP. Temporary radiation-induced alopecia after embolization of a cerebral arteriovenous malformation. Clin Exp Dermatol. 2015; 40(1): 88-90. doi: 10.1016/ s0303-8467(03)00007-6.
Rao SB. Biological bases for the revision of dose limits to the eye lens. J Med Phys. 2016; 41(4): 211–3. doi: 10.4103/0971-6203.195183.
Matsubara K, Yoshida S, Hirosawa A, Chusin T, Furukawa Y. Characterization of small dosimeters used for measurement of eye lens dose for medical staff during fluoroscopic examination. Diagnostics. 2021; 11(2): 150. doi: 10.3390/diagnostics11020150.
D D’Alessio A, Matheoud R, Cannillo B, Guzzardi G, Galbani F, Galbiati A, Spinetta M, Stanca C, Tettoni SM, Carriero A, Brambilla M. Evaluation of operator eye exposure and eye protective devices in interventional radiology: Results on clinical staff and phantom. Phys Med. 2023; 110: 102603. doi: 10.1016/j.ejmp.2023.102603.
Mussmann B, Larsen TR, Godballe M, Abdi AJ, Kantsø A, Jakobsen AR, Nielsen MV, Jensen J. Radiation dose to multidisciplinary staff members during complex interventional procedures. Radiography (Lond). 2024; 30(2): 512-6. doi: 10.1016/j.radi.2024.01.010.
Somtom T, Somboot T, Awikunprasert P, Kittichotwarat S, Damchoo P, Mongkolratnan A, et al. Radiation dose in radiologist from cerebral angiography using optically stimulated luminescence dosimeter. J Assoc Med Sci. 2024; 57(1): 29-37. doi: 10.12982/JAMS. 2024.004.
Kim JH. Three principles for radiation safety: time, distance, and shielding. Korean J Pain. 2018; 31(3): 145-6. doi: 10.3344/kjp.2018.31.3.145.
Alhasan AS, Aalam WA. Eye lens opacities and cataracts among physicians and healthcare workers occupationally exposed to radiation: A systematic review and meta- analysis. Saudi Med J. 2022; 43(7): 665-77. doi: 10.15537/smj.2022.43.7.20220022.
Rose A, Rae WID, Sweetlove MA, Ngetu L, Benadjaoud MA, Marais W. Radiation induced cataracts in interventionalists occupationally exposed to ionising radiation. SA J Radiol. 2022; 26(1): 2495. doi: 10.4102/ sajr.v26i1.2495.
Shubayr N, Alashban Y. Medical occupational dose to the skin based on Hp(0.07) measured by thermoluminescent dosimeter: A Saudi nationalstudy. Radiat Phys Chem. 2022; 201: 110439. doi: 10.1016/j.radphyschem.2022.110439.
Nupetch S, Awikunprasert P, Pungkun V. Radiation dose response of InLight® optically stimulated luminescence (OSL) dosimeter. Thai J Radiol Technol. 2018; 43(1): 36-43.