COVID-19 vaccination doesn’t influence sperm motility, concentration, and morphology
Main Article Content
Abstract
Background: The COVID-19 pandemic, driven by SARS-CoV-2, necessitated the rapid development and global deployment of vaccines. Despite the high efficacy of vaccines like AstraZeneca and Pfizer-BioNTech in preventing severe COVID-19, concerns about potential side effects, particularly on male fertility, have arisen.
Objective: This study aims to evaluate the impact of COVID-19 vaccination on key sperm parameters (motility, concentration, count, and morphology) and serum interleukin-6 (IL-6) levels in men.
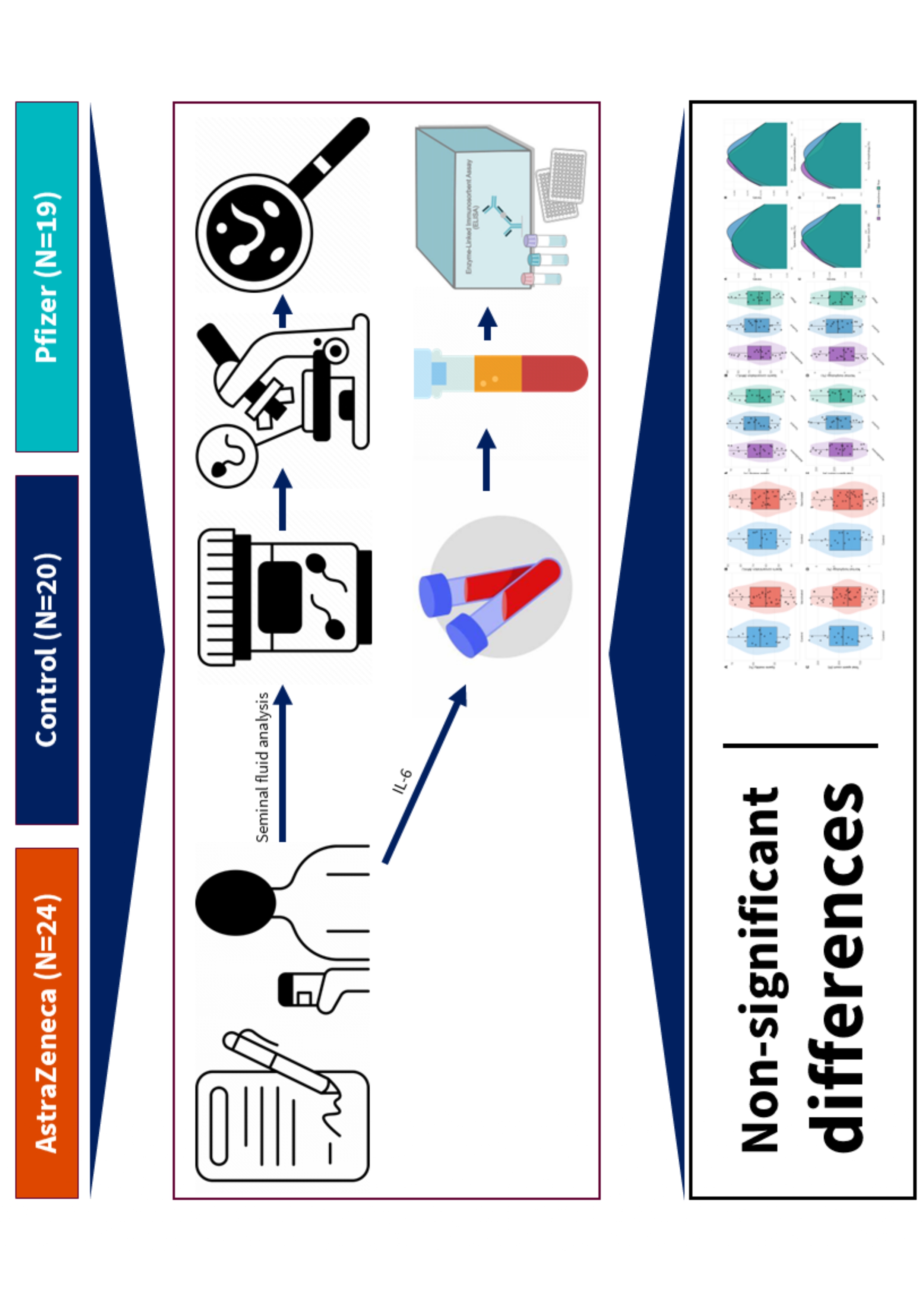
Materials and methods: A cross-sectional study was conducted over six months (March to August 2022) at the High Institute for Infertility Diagnosis and Assisted Reproductive Technologies in Baghdad, Iraq. The study included 63 participants divided into three groups: AstraZeneca vaccine group (N=24), Pfizer vaccine group (N=19), and an unvaccinated control group (N=20). Participants’ sperm parameters were analyzed following the WHO guidelines, and serum IL-6 levels were measured using ELISA.
Results: No statistically significant differences were found in sperm motility, concentration, total sperm count, or morphology between vaccinated and unvaccinated groups. Specifically, sperm motility was 57.3±8.9% in the vaccinated group versus 56.8±9.2% in the control group (p=0.782). Sperm concentration was 62.5±14.7 M/mL in the vaccinated group compared to 61.9±15.1 M/mL in the control group (p=0.845). Total sperm count was 185.6±43.8 M in the vaccinated group versus 183.2±44.5 M in the control group (p=0.802). Morphologically normal sperm were 4.2±1.1% in the vaccinated group versus 4.1±1.0% in the control group (p=0.659). Serum IL-6 levels showed no significant differences between the groups.
Conclusion: COVID-19 vaccination with either AstraZeneca or Pfizer-BioNTech does not adversely affect sperm parameters or induce significant changes in serum IL-6 levels. These findings support the safety of COVID-19 vaccines concerning male reproductive health, alleviating concerns about potential adverse effects on fertility.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. 2020; 382(8): 727-33. doi: 10.1056/ NEJMoa2001017
Luay A, Mohsen Al-Essawe E, Al-Kawaz U. Prevalence of erectile dysfunction in males post COVID-19 infection. Iraqi J Embryos Infertil Res. 2021; 11(1): 89-98. Available from: https://ijeir.net/index.php/ ijeir/article/view/70
Chandramouli T, Mishra SB, Rath A. Reinfection of SARS CoV-2 in patients with relapse of symptoms after clinical recovery: A case series. J Assoc Med Sci. 2022; 55(3): 105-8. Available from: https:// he01.tci-thaijo.org/index.php/bulletinAMS/article/ download/255037/174080
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020; 383(27): 2603-15. doi/10.1056/NEJMoa2034577
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021; 397(10269): 99-111. Available from: https://linkinghub.elsevier.com/retrieve/pii/ S0140673620326611
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021; 384(5):403- 16. doi/10.1056/NEJMoa2035389
Diaz P, Reddy P, Ramasahayam R, Kuchakulla M, Ramasamy R. COVID-19 vaccine hesitancy linked to increased internet search queries for side effects on fertility potential in the initial rollout phase following Emergency Use Authorization. Andrologia. 2021; 53(9):e14156. doi/10.1111/and.14156
Roozenbeek J, Schneider CR, Dryhurst S, Kerr J, Freeman ALJ, Recchia G, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci. 2020; 7(10): 201199. doi/10.1098/ rsos.201199
Wang Z, Xu X. scRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in spermatogonia, Leydig and Sertoli cells. Cells. 2020; 9(4): 920. Available from: https://www.mdpi.com/2073-4409/9/4/920
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med. 2001; 345(19): 1388-93. doi/ abs/10.1056/NEJMoa003005
Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HWG, Behre HM, et al. World Health Organization reference values for human semen characteristics*‡. Hum Reprod Update. 2010; 16(3):231-45. Available from: http://academic.oup. com/humupd/article/16/3/231/639175/WorldHealth-Organization-reference-values-for
Moretti E, Cosci I, Spreafico A, Serchi T, Cuppone AM, Collodel G. Semen characteristics and inflammatory mediators in infertile men with different clinical diagnoses. Int J Androl. 2009; 32(6): 637-46. doi/10.1111/j.1365-2605.2008.00911.x
Erbay G, Sanli A, Turel H, Yavuz U, Erdogan A, Karabakan M, et al. Short‐term effects of COVID‐19 on semen parameters: A multicenter study of 69 cases. Andrology. 2021;9(4): 1060-5. doi/10.1111/ andr.13019
Gacci M, Coppi M, Baldi E, Sebastianelli A, Zaccaro C, Morselli S, et al. Semen impairment and occurrence of SARS-CoV-2 virus in semen after recovery from COVID-19. Hum Reprod. 2021; 36(6):1520-9. Available from: https://academic.oup.com/humrep/ article/36/6/1520/6125160
Gonzalez DC, Nassau DE, Khodamoradi K, Ibrahim E, Blachman-Braun R, Ory J, et al. Sperm parameters before and after COVID-19 mRNA vaccination. JAMA. 2021; 326(3): 273-4. doi: 10.1001/jama.2021. 9976
Barda S, Laskov I, Grisaru D, Lehavi O, Kleiman S, Wenkert A, et al. The impact of COVID‐19 vaccine on sperm quality. Int J Gynecol Obstet. 2022; 158(1): 116-20. doi/10.1002/ijgo.14135
Li H, Xiao X, Zhang J, Zafar MI, Wu C, Long Y, et al. Impaired spermatogenesis in COVID-19 patients. EClinicalMedicine. 2020; 28:100604. Available from: https://linkinghub.elsevier.com/retrieve/pii/ S2589537020303485
Navarra A, Albani E, Castellano S, Arruzzolo L, Levi-Setti PE. Coronavirus disease-19 infection: Implications on male fertility and reproduction. Front Physiol. 2020; 11. Available from: https://www.frontiersin.org/ articles/10.3389/fphys.2020.574761/full
Qian L, Sun G, Zhou B, Wang G, Song J, He H. Study on the relationship between different cytokines in the semen of infertility patients. Am J Reprod Immunol. 2011; 66(2): 157-61. doi/10.1111/j.1600- 0897.2010.00980.x