Effect of a multisensory integration intervention on policewomen with migraine
Main Article Content
Abstract
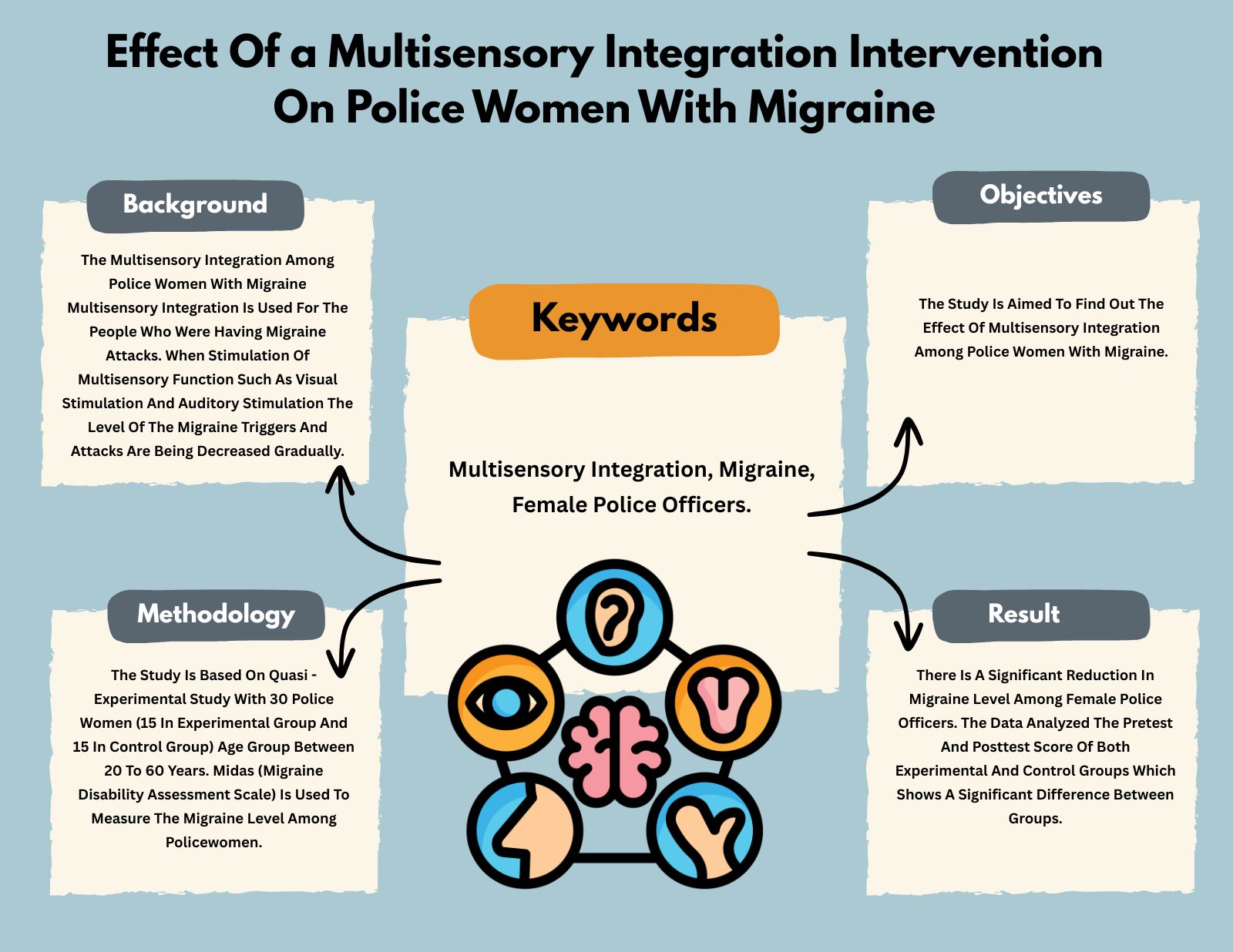
Background: Multisensory integration is used for people who are having migraine attacks. When multisensory functions such as visual and auditory stimulation are applied, the level of migraine triggers and attacks decreases gradually.
Objectives: The study aimed to determine the effect of multisensory integration intervention on policewomen with migraine.
Materials and methods: The study is based on a quasi-experimental study with 30 policewomen (15 in the experimental group and 15 in the control group) aged between 20 and 60. The MIDAS (Migraine Disability Assessment Scale) was used to measure the migraine level among policewomen.
Results: There is a significant reduction in migraine levels among female police officers. The data shows that the pre-test and post-test scores of both experimental and control groups were significantly different. Since the p value is lesser than 0.05, alternate hypothesis is accepted. Hence, there is a statistically significant difference in post-test scores between experimental and control group. This suggests that the intervention received by the experimental group had greater improvement when compared to the control group.
Conclusion: Multisensory integration has a significant effect on reducing migraines among female police officers. This study’s benefit is to reduce the impact of migraines on individuals through multisensory integration-based activities.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Amiri P, Kazeminasab S, Nejadghaderi SA, Mohammadinasab R, Pourfathi H, Araj-Khodaei M, et al. Migraine: A review on its history, global epidemiology, risk factors, and comorbidities. Front Neurol. 2022; 12: 800605. doi: 10.3389/fneur.2021.800605.
Haghdoost F, Togha M. Migraine management: Non-pharmacological points for patients and health care professionals. Open Med. 2022; 17(1): 1869-82. doi: 10.1515/med-2022-0598.
De Dhaem OB, Sakai F. Migraine in the workplace. Neurol Sci. 2022; 27: 100408. doi: 10.1016/j.ensci. 2022.100408.
Stein BE, Stanford TR, Rowland BA. Development of multisensory integration from the perspective of the individual neuron. Nat Rev Neurosci. 2014; 15(8): 520-35. doi: 10.1038/nrn3742.
Buse DC, Rupnow MFT, Lipton RB. Assessing and managing all aspects of migraine: migraine attacks, migraine-related functional impairment, common comorbidities, and quality of life. Mayo Clin Proc. 2009; 84(5): 422-35. doi: 10.1016/s0025-6196(11)60561-2.
Leso V, Gervetti P, Mauro S, Macrini MC, Ercolano ML, Iavicoli I. Shift work and migraine: A systematic review. Occup Health. 2020; 62(1): e12116. doi: 10.1136/ bmjopen-2013-002791.
Garbarino S, Cuomo G, Chiorri C, Magnavita N. Association of work-related stress with mental health problems in a special police force unit. BMJ Open. 2013; 3(7): e002791. doi: 10.1136/bmjopen-2013- 002791.
Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) questionnaire to assess headache- related disability. Neurology. 2001; 56(Suppl 1): S20-8. doi: 10.1212/wnl.56.suppl_1.s20
Peng KP, Wang SJ. Migraine diagnosis: Screening items, instruments, and scales. Acta Anaesthesiol Taiwan. 2012; 50(2): 69-73. doi: 10.1016/j.aat.2012.05.002.
Philips EG. Exploring occupational therapy’s role in headache & migraine management for women in military aviation fields through a biopsychosocial approach. Boston (MA): Boston University; 2023.
Schwedt TJ. Chronic migraine. BMJ. 2014; 348: g1416. doi: 10.1136/bmj.g1416.