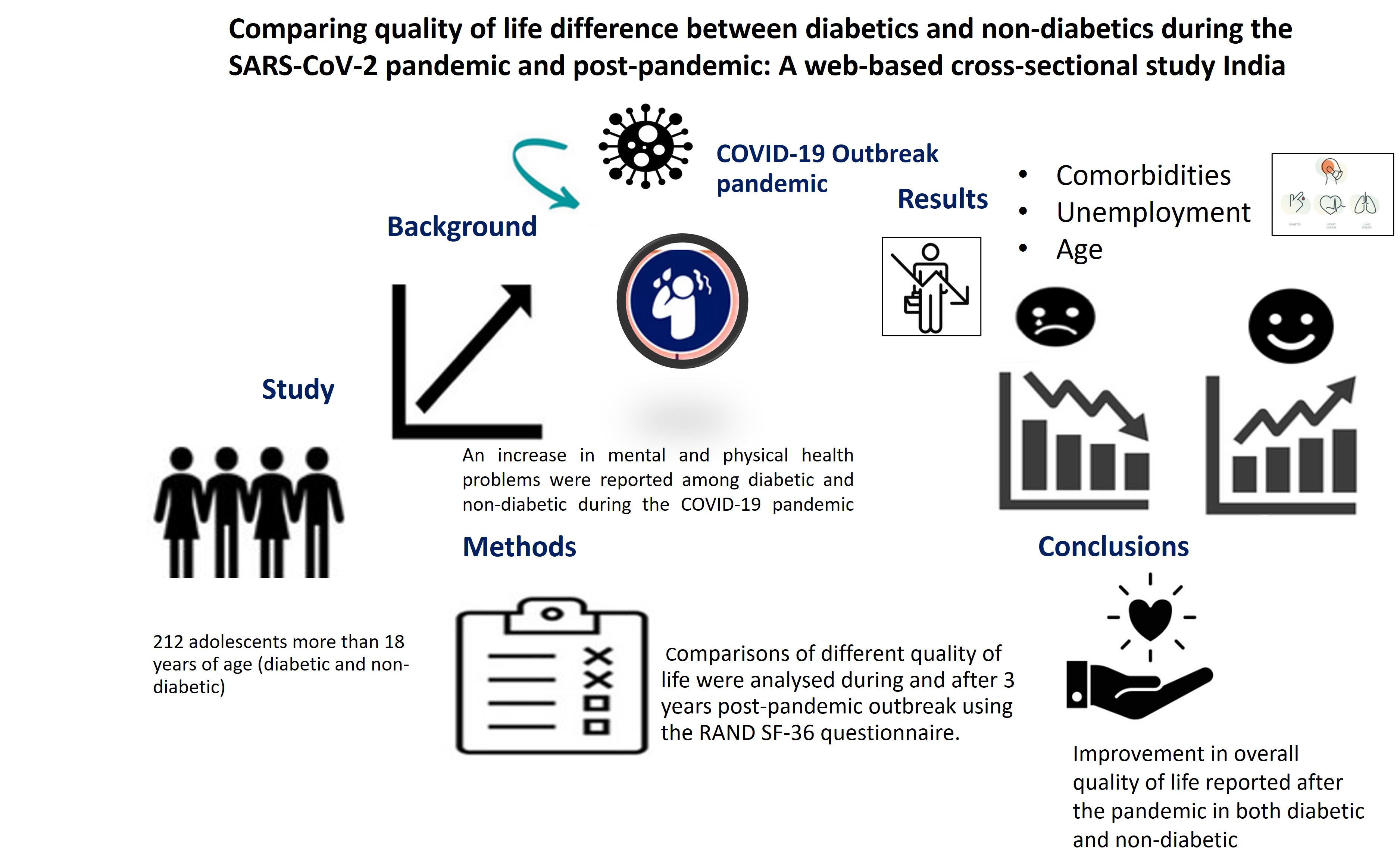
Comparing quality of life difference between diabetics and non-diabetics during the SARS-CoV-2 pandemic and post-pandemic: A web-based cross-sectional study India
Main Article Content
Abstract
Background: The COVID-19 pandemic has irreversibly altered the global landscape, with far-reaching consequences for individuals’ quality of life (QOL). In India, the series of lockdowns imposed to combat the pandemic presented unique challenges, exacerbating mental health concerns and amplifying anxiety and discontent among the population. Notably, the pandemic’s impact on QOL has been unevenly distributed, with diabetic individuals potentially facing distinct challenges compared to their non-diabetic counterparts. Existing research in India has primarily focused on the health-related concerns of diabetic individuals, leaving a significant knowledge gap regarding the QOL of non-diabetic individuals during and following the pandemic. A comprehensive understanding of QOL differences between diabetic and non-diabetic populations is crucial for developing targeted interventions and improving overall well-being.
Objective: This study aims to address this gap by exploring and comparing the QOL of diabetic and non-diabetic individuals in India during and after COVID-19, providing valuable insights into the pandemic’s impact on this critical aspect of health.
Materials and methods: A cross-sectional, comparative online-based survey study was conducted among 212 participants (diabetic and non-diabetic) aged 18 years and below 60 years visiting SRM General Hospital, between July and August 2021 during the COVID-19, and their self-reported scores were compared two years post-pandemic. A snowball sampling method was employed due to the pandemic's dynamic nature and online data collection feasibility. The RAND SF-36, a widely used 36-item quality-of-life questionnaire, was administered online via Google Forms and distributed through social media platforms and email invitations. Paired t-tests compared quality of life (QOL) during and after the SARS-CoV-2 pandemic. Multivariate regression analysis identified independent predictors influencing RAND SF-36 subscale scores.
Results: The study involved the collection of responses from a total of 212 participants, with a mean age of 46.61±17.4 years. The RAND SF-36 questionnaire assessed the quality of life (QOL) during and after the SARS-CoV-2 pandemic. The results revealed significant differences in the general (45.8±13.0 vs 64.9±19.7; p=0.001) and mental health (53.5±12.3vs. 62.7±12.8, p<0.001) between the two time periods.Furthermore, the study revealed age (β=-0.369, p=0.004, 95%CI [-0.608, -0.101]) and employment status(β=-2.11, p=0.041, 95%CI [ -0.083, -4.139]) showed significant negative association with physical health-related component. In addition, the duration of comorbidities (β=-5.326, p=0.047,95%CI [-11.408, -0.756] gravely affected the mental health component, respectively.>
Conclusion: Significant differences were noted in quality of life (QOL) between the SARS-CoV-2 pandemic period and after, with lower general health and mental health scores shown in diabetics as compared to non-diabetic individuals. Older age and unemployment were associated with worse physical health QoL, while the longer duration of comorbidities negatively impacted mental health QOL regardless of diabetes status. These findings suggest the pandemic substantially affected various aspects of QoL, underscoring the need for targeted interventions to support vulnerable populations.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
World Health Organization. COVID-19 significantly impacts health services for noncommunicable diseases. Retrived 2024 November 13. Available from: https://www.who.int/news/item/01-06-2020- covid-19-significantly-impacts-health-services-fornoncommunicable-diseases
Ministry of Health and Family Welfare. Government of India. Retrived 2024 November 13. Available from: https://mohfw.gov.in/
Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi: 10.1183/13993003.00547-2020
Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, et al. The increasing burden of diabetes and variations among the states of India: the Global Burden of Disease Study 1990-2016. The Lancet Global Health. 2018 ; 6(12): e1352-62. doi: 10.1016/S2214- 109X(18)30387-5
Kumar A, Arora A, Sharma P, Anikhindi SA, Bansal N, Singla V, et al. Clinical Features of COVID-19 and Factors Associated with Severe Clinical Course: A Systematic Review and Meta-analysis. SSRN. 2020; 3566166. doi: 10.2139/ssrn.3566166
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020; 94: 91-5. doi: 10.1016/j.ijid.2020.03.017
Huang I, Lim MA, Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia - A systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020; 14(4): 395-403. doi: 10.1016/j.dsx.2020. 04.018
Singh AK, Singh R. Does poor glucose control increase the severity and mortality in patients with diabetes and COVID-19? Diabetes Metab Syndr. 2020; 14(5): 725-7.doi: 10.1016/j.dsx.2020.05.037
Ghosal S, Bhattacharyya R, Majumder M. Impact of complete lockdown on total infection and death rates: A hierarchical cluster analysis. Diabetes Metab Syndr. 2020; 14(4): 707. doi: 10.1016/j.dsx.2020.05.026
Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr. 2020; 14(5): 917-20. doi: 10.1016/j.dsx.2020.05.044
Verma A, Rajput R, Verma S, Balania VKB, Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 Diabetes Mellitus. Diabetes Metab Syndr. 2020; 14(5): 1213-6. doi: 10.1016/j. dsx.2020.07.016
Khan AG, Kamruzzaman Md, Rahman MdN, Mahmood M, Uddin MdA. Quality of life in the COVID-19 outbreak: influence of psychological distress, government strategies, social distancing, and emotional recovery. Heliyon. 2021; 7(3): e06407.doi: 10.1016/j.heliyon. 2021.e06407
Zhang Y, Ma ZF. Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int J Environ Res Public Health. 2020; 17(7): 2381. doi:10.3390/ijerph17072381
Eysenbach G, Wyatt J. Using the Internet for surveys and health research. J Med Internet Res. 2002; 4(2): E13. doi: 10.2196/jmir.4.2.e13 [15] Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ : Br Med J. 1992; 305(6846): 160. doi: 10.1136/bmj.305.6846.160
Gandek B, Ware JE, Aaronson NK, Alonso J, Apolone G, Bjorner J, et al. Tests of data quality, scaling assumptions, and reliability of the SF-36 in eleven countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998; 51(11): 1149-58. doi: 10.1016/s0895-4356(98)00106-1
Sinha R, van den Heuvel WJA, Arokiasamy P. Validity and Reliability of MOS Short Form Health Survey (SF- 36) for Use in India. Indian J Community Med. 2013; 38(1): 22-6. doi: 10.4103/0970-0218.106623
Kohli RM, Sane S, Kumar K, Paranjape RS, Mehendale SM. Assessment of quality of life among HIV-infected persons in Pune, India. Qual Life Res. 2005; 14(6): 1641-7. doi: 10.1007/s11136-004-7082-8
RAND Medical Outcomes Study. 36-Item Short Form Survey. Santa Monica, CA: RAND Corporation. Retrived 2024 June 3. Availablefrom: https://www. rand.org/healthcare/surveys_tools/mos/36-itemshort-form.html
Hays RD, Sherbourne CD, Mazel RM. The RAND 36- Item Health Survey 1.0. Health Econ. 1993; 2(3): 217- 27. doi: 10.1002/hec.4730020305
Al-Sofiani ME, Albunyan S, Alguwaihes AM, Kalyani RR, Golden SH, Alfadda A. Determinants of mental health outcomes among people with and without diabetes during the COVID-19 outbreak in the Arab Gulf Region. J Diabetes. 2021; 13(4): 339-52. doi: 10.1111/1753-0407.13149
Badinlou F, Rahimian F, Hedman-Lagerlöf M, Lundgren T, Abzhandadze T, Jansson-Fröjmark M. Trajectories of mental health outcomes following COVID-19 infection: a prospective longitudinal study. BMC Public Health. 2024; 24(1): 452. doi: 10.1186/s12889-024-17997-x
Meher D, Kar S. Effect of pandemic on Quality of life in Diabetics (QOLID) assessment: Data from a teaching hospital in Bhubaneswar, Odisha, India. J Fam Med Prim Care. 2021; 10(10): 3780. doi: 10.4103/jfmpc. jfmpc_287_21
Ayalew M, Deribe B, Hussen S, Defar S, Gedefaw A. Quality of life among patients with chronic noncommunicable diseases during COVID-19 pandemic in Southern Ethiopia: A cross-sectional analytical study. Front Psychiatry. 2022; 13: 855016.doi: 10.3389/fpsyt.2022.855016
Aschalew AY, Yitayal M, Minyihun A. Health-related quality of life and associated factors among patients with diabetes mellitus at the University of Gondar referral hospital. Health Qual Life Outcomes. 2020; 18(1): 62. doi: 10.1186/s12955-020-01311-5
Khorani H, Mohammadi F, Hosseinkhani Z, Motalebi SA. Predictive factors of Quality of Life in older adults during the COVID-19 pandemic. BMC Psychol. 2022; 10(1): 176. doi: 10.1186/s40359-022-00882-w
Romero Starke K, Petereit-Haack G, Schubert M, Kämpf D, Schliebner A, Hegewald J, et al. The AgeRelated Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and MetaRegression. Int J Environ Res Public Health. 2020; 17(16): 5974. doi: 10.3390/ijerph17165974
Zhang SX, Wang Y, Rauch A, Wei F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020; 288: 112958. doi: 10.1016/j.psychres.2020.112958
Khan MdAS, Dalal K, Hasan M, Haque MMdA, NusratE-Mozid, Hossian M, et al. The impact of comorbidity on the quality of life of people who recovered from COVID-19 in Bangladesh. IJID Regions. 2024; 11: 100351. doi: 10.1016/j.ijregi.2024.03.006