Analyzing dprE1 gene variations in drug-resistant Mycobacterium tuberculosis isolates from Northern Thailand
Main Article Content
Abstract
Background: DprE1 has been discovered as a highly promising candidate for eradicating multidrug-resistant tuberculosis (MDR-TB) due to its localization and crucial role in cell wall synthesis. Several DprE1 inhibitors in clinical trials target different binding sites on the DprE1 protein. However, mutations in these binding sites can result in resistance to these inhibitors. Nonetheless, only a few reports exist on the sequence analysis of the dprE1 gene in drug-resistant clinical isolates, especially in Thailand, a country with a high TB burden.
Objective: To investigate the genetic variations in the dprE1 gene among drugresistant clinical Mycobacterium tuberculosis (Mtb) isolates from Northern Thailand and to examine mutations known to confer resistance to specific inhibitors.
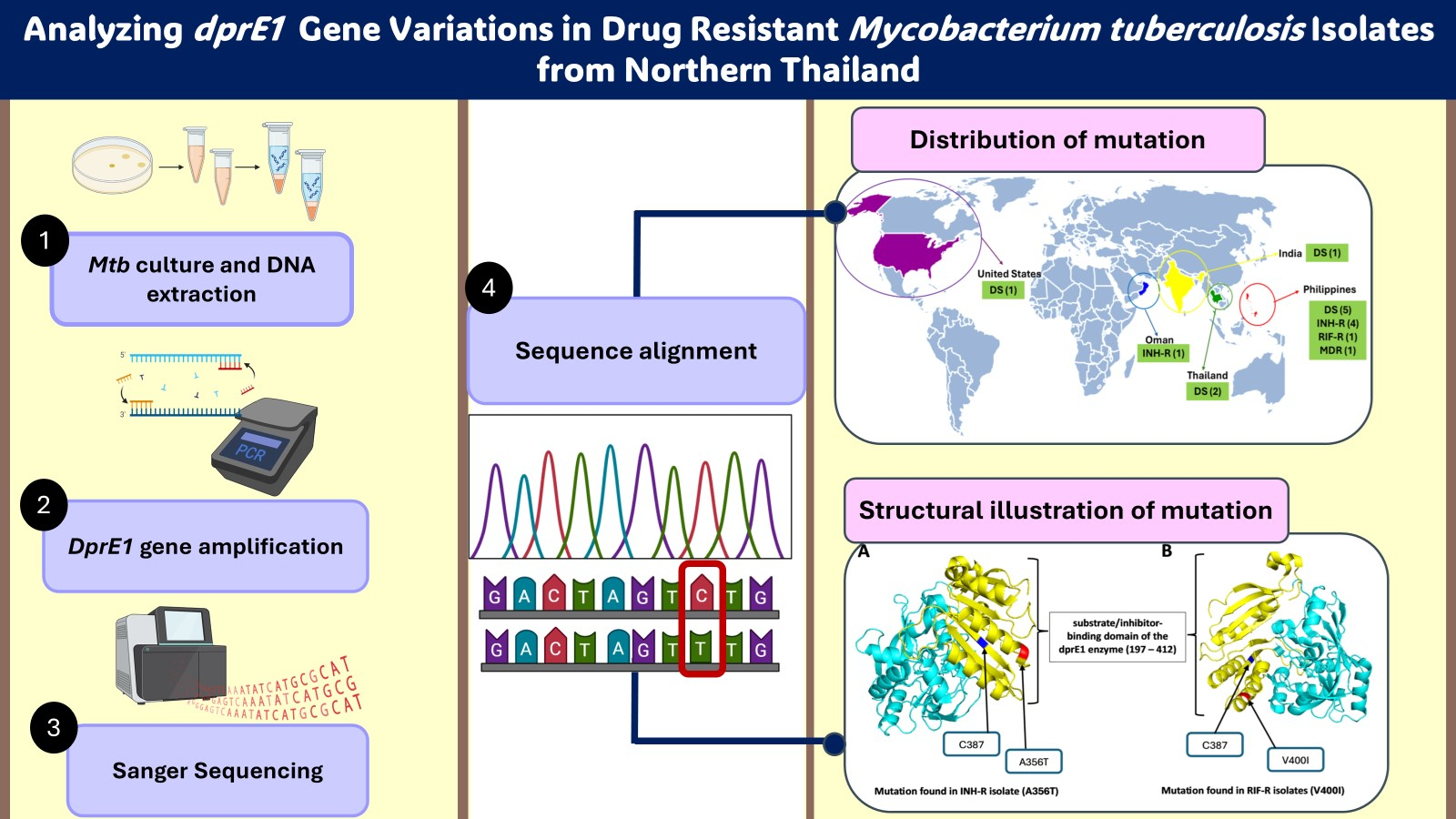
Materials and methods: Drug resistance profiles of 19 clinical Mtb isolates from Northern Thailand—11 multidrug-resistant Mtb, 2 isoniazid-resistant Mtb, and 6 rifampicin-resistant Mtb-were assessed using the agar proportion method and Sanger sequencing. New PCR and sequencing primers were designed to cover the entire length of the dprE1 gene. Mutation profiles were detected by performing DNA alignment against the reference strain, M. tuberculosis H37Rv, using BioEdit Sequence Alignment version 7.2.5. The distribution of these mutations was assessed through the Basic Local Alignment Search Tool (BLAST) server. Visual representation of amino acid mutation regions in DprE1 was generated using the PyMOL 3.0.
Results: The mutation at codon 387 associated with benzothiazinone (BTZ) compounds was not observed in the dprE1 gene of any clinical isolates. The most common mutation profile, C→T at codon 459, was found in 73.68% of clinical isolates. However, this is a silent mutation and probably indicates genetic polymorphism. Non-synonymous substitutions in the dprE1 gene were detected: A356T in one INH-R isolate and V400I in two RIF-R isolates. BLAST analysis revealed that the A356T mutation in the INH-R isolates had a 100% match with sixteen Mtb strains from other regions. Interestingly, the V400I mutation in the RIF-R isolates had not been reported, making this the first documentation of such a finding.
Conclusion: Although no mutations directly linked to resistance against current DprE1 inhibitors were found, mutations in the DprE1 binding sites could affect the efficacy of these inhibitors. This study highlights the significance of mono-drugresistant strains that acquire dprE1 mutations, potentially complicating future TB treatment targeting DprE1.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Bagcchi S. WHO’s Global Tuberculosis Report 2022. Lancet Microbe. 2023; 4(1): e20.
doi: 10.1016/S2666- 5247(22)00359-7
Dash S, Rathi E, Kumar A, Chawla K, Kini SG. Identification of DprE1 inhibitors for tuberculosis through integrated in-silico approaches. Sci Rep. 2024; 14(1): 11315. doi: 10.1038/s41598-024-61901-x
de Steenwinkel JE, ten Kate MT, de Knegt GJ, Verbrugh HA, Aarnoutse RE, Boeree MJ, et al. Consequences of noncompliance for therapy efficacy and emergence of resistance in murine tuberculosis caused by the Beijing genotype of Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2012; 56(9): 4937-44. doi: 10.1128/AAC.00124-12
Dash S, Rathi E, Kumar A, Chawla K, Joseph A, Kini SG. Structure-activity relationship mediated molecular insights of DprE1 inhibitors: A Comprehensive Review. J Biomol Struct Dyn. 2024; 42(12): 6472-522. doi: 10.10 80/07391102.2023.2230312
Gandhi NR, Nunn P, Dheda K, Schaaf HS, Zignol M, van Soolingen D, et al. Multidrug-resistant and extensively drug-resistant tuberculosis: a threat to global control of tuberculosis. Lancet. 2010; 375(9728): 1830-43. doi: 10.1016/S0140-6736(10)60410-2
Jacobo-Delgado YM, Rodríguez-Carlos A, Serrano CJ, Rivas-Santiago B. Mycobacterium tuberculosis cell-wall and antimicrobial peptides: a mission impossible? Front Immunol. 2023; 14:1194923. doi: 10.3389/fimmu. 2023.1194923
Riccardi G, Pasca MR, Chiarelli LR, Manina G, Mattevi A, Binda C. The DprE1 enzyme, one of the most vulnerable targets of Mycobacterium tuberculosis. Appl Microbiol Biotechnol. 2013; 97(20): 8841-8. doi: 10.1007/s00253-013-5218-x
Chen K, Xu R, Hu X, Li D, Hou T, Kang Y. Recent advances in the development of DprE1 inhibitors using AI/CADD approaches. Drug Discov Today. 2024;29(6):103987. doi: 10.1016/j.drudis.2024.103987 [9] Brennan PJ, Nikaido H. The envelope of mycobacteria. Annu Rev Biochem. 1995; 64: 29-63.
doi: 10.1146/ annurev.bi.64.070195.000333
Piton J, Foo CS, Cole ST. Structural studies of Mycobacterium tuberculosis DprE1 interacting with its inhibitors. Drug Discov Today. 2017; 22(3): 526- 33. doi: 10.1016/j.drudis.2016.09.014
Yadav S, Soni A, Tanwar O, Bhadane R, Besra GS, Kawathekar N. DprE1 Inhibitors: Enduring aspirations for future antituberculosis drug discovery. ChemMedChem. 2023; 18(16): e202300099. doi: 10.1002/cmdc. 202300099
Shi J, Lu J, Wen S, Zong Z, Huo F, Luo J, et al. In Vitro Activity of PBTZ169 against multiple Mycobacterium species. Antimicrob Agents Chemother. 2018; 62(11) :e01314-18.
doi: 10.1128/AAC.01314-18
Fil M, Alibert S. Unveiling DprE1 as a Key Target in the Fight against Tuberculosis: Insights and perspectives on developing novel antimicrobial agents. BioMed. 2024; 4(3): 220-36.
doi: 10.3390/biomed4030018
Incandela ML, Perrin E, Fondi M, de Jesus Lopes Ribeiro AL, Mori G, Moiana A, et al. DprE1, a new taxonomic marker in mycobacteria. FEMS Microbiol Lett. 2013; 348(1): 66-73. doi: 10.1111/1574-6968.12246
Pasca MR, Degiacomi G, Ribeiro AL, Zara F, De Mori P, Heym B, et al. Clinical isolates of Mycobacterium tuberculosis in four European hospitals are uniformly susceptible to benzothiazinones. Antimicrob Agents Chemother. 2010; 54(4): 1616-8. doi: 10.1128/AAC. 01676-09
Saikaew S, Thongprachum A, Pongsararuk R, Thanraka A, Kunyanone N, Chaiyasirinroje B, et al. Genotypic distribution and the epidemiology of multidrug resistant tuberculosis in Upper Northern Thailand. Antibiotics (Basel). 2022; 11(12): 1733. doi: 10.3390/ antibiotics11121733
Yimcharoen M, Saikaew S, Wattananandkul U, Phunpae P, Intorasoot S, Kasinrerk W, et al. The regulation of ManLAM-related gene expression in Mycobacterium tuberculosis with different drug resistance profiles following isoniazid treatment. Infect Drug Resist. 2022; 15: 399-412.
doi: 10.2147/IDR.S346869
Amado PSM, Woodley C, Cristiano MLS, O’Neill PM. Recent advances of DprE1 inhibitors against Mycobacterium tuberculosis: Computational analysis of physicochemical and ADMET properties. ACS Omega. 2022; 7(45): 40659-81. doi: 10.1021/acsomega.2c05307
Yadav P. Challenges & solutions for recent advancements in multi-drugs resistance tuberculosis: A Review. Microbiol Insights. 2023; 16: 11786361231152438. doi: 10.1177/11786361231152438
Kolly GS, Boldrin F, Sala C, Dhar N, Hartkoorn RC, Ventura M, et al. Assessing the essentiality of the decaprenylphospho-d-arabinofuranose pathway in Mycobacterium tuberculosis using conditional mutants. Mol Microbiol. 2014; 92(1): 194-211. doi: 10.1111/mmi.12546
Poulton NC, Azadian ZA, DeJesus MA, Rock JM. Mutations in rv0678 confer low-Level resistance to benzothiazinone DprE1 inhibitors in Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2022; 66(9): e0090422. doi: 10.1128/aac.00904-22
Gygli SM, Borrell S, Trauner A, Gagneux S. Antimicrobial resistance in Mycobacterium tuberculosis: mechanistic and evolutionary perspectives. FEMS Microbiol Rev. 2017; 41(3): 354-73. doi: 10.1093/femsre/fux011
Kimchi-Sarfaty C, Oh JM, Kim IW, Sauna ZE, Calcagno AM, Ambudkar SV, et al. A “silent” polymorphism in the MDR1 gene changes substrate specificity. Science. 2007; 315(5811): 525-8.
doi: 10.1126/science. 1135308
Finger V, Kucera T, Kafkova R, Muckova L, Dolezal R, Kubes J, et al. 2,6-Disubstituted 7-(naphthalen-2-ylmethyl)-7H-purines as a new class of potent antitubercular agents inhibiting DprE1. Eur J Med Chem. 2023; 258: 115611. doi: 10.1016/j.ejmech.2023. 115611
Ezquerra-Aznárez JM, Degiacomi G, Gašparovič H, Stelitano G, Sammartino JC, Korduláková J, et al. The veterinary anti-parasitic selamectin is a novel inhibitor of the Mycobacterium tuberculosis DprE1 Enzyme. Int J Mol Sci. 2022; 23(2): 771. doi: 10.3390/ ijms23020771
Makarov V, Manina G, Mikusova K, Möllmann U, Ryabova O, Saint-Joanis B, et al. Benzothiazinones kill Mycobacterium tuberculosis by blocking arabinan synthesis. Science. 2009; 324(5928): 801-4. doi: 10. 1126/science.1171583
Jugheli L, Bzekalava N, de Rijk P, Fissette K, Portaels F, Rigouts L. High level of cross-resistance between kanamycin, amikacin, and capreomycin among Mycobacterium tuberculosis isolates from Georgia and a close relation with mutations in the rrs gene. Antimicrob Agents Chemother. 2009; 53(12): 5064-8. doi: 10.1128/AAC.00851-09
Bergval I, Kwok B, Schuitema A, Kremer K, van Soolingen D, Klatser P, et al. Pre-existing isoniazid resistance, but not the genotype of Mycobacterium tuberculosis drives rifampicin resistance codon preference in vitro. PLoS One. 2012; 7(1): e29108. doi: 10.1371/journal. pone.0029108
Torres Ortiz A, Coronel J, Vidal JR, Bonilla C, Moore DAJ, Gilman RH, et al. Genomic signatures of preresistance in Mycobacterium tuberculosis. Nat Commun. 2021; 12(1): 7312. doi: 10.1038/s41467-021-27616-7