Improvement in Neisseria gonorrhoeae culture using modified fastidious broth
Main Article Content
Abstract
Background: Culture of Neisseria gonorrhoeae is essential for antimicrobial susceptibility testing and drug resistance surveillance. However, the success rate for N. gonorrhoeae culture from samples collected at sexually transmitted disease clinics is low. Moreover, culturing this fastidious organism can be challenging.
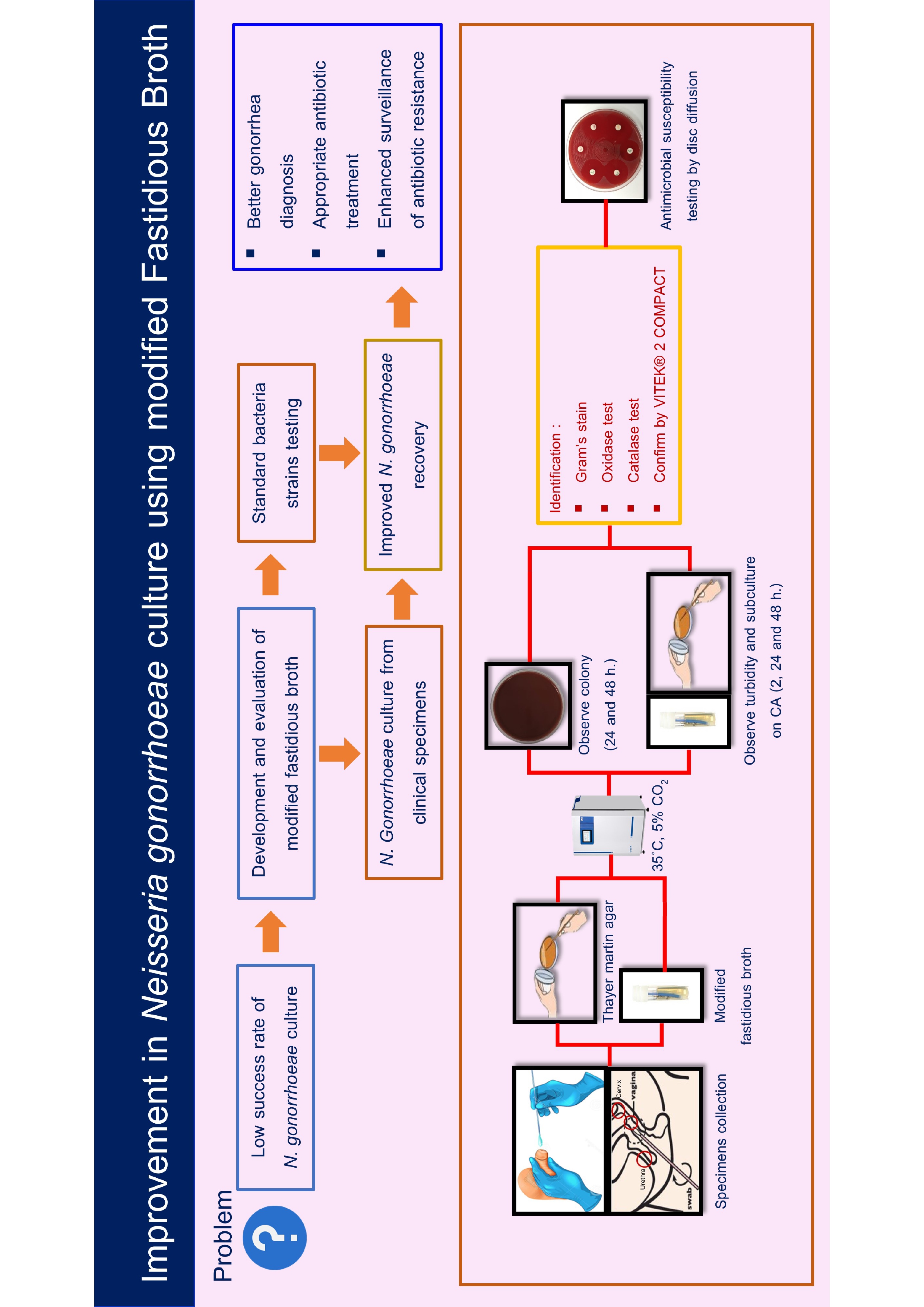
Objective: This study aimed to develop and evaluate a modified fastidious broth (mFB) for improved preservation and culture of N. gonorrhoeae that would serve as both a transport medium for specimen collection from patients with suspected gonococcal infections and a growth enhancer for N. gonorrhoeae culture.
Materials and methods: The mFB was evaluated using five standard bacteria strains at a concentration of 105 , 103 , and 101 CFU/ml: N. gonorrhoeae, Streptococcus agalactiae, Listeria monocytogenes, Escherichia coli, and Staphylococcus saprophyticus. After that, the mFB was used to collect specimens from 29 patients (77 samples) at the Venereal Disease Clinic at Mae Sot Hospital in Tak Province, Thailand, between October 2023 and February 2024. A total of 77 specimens were divided into 2 groups according to the gram-negative diplococci in Gram stain: 1) positive results (8 specimens) and 2) negative results (69 specimens). Furthermore, the N. gonorrhoeae culture was compared by using mFB on Chocolate agar (CA) and the direct plate specimen culture on Thayer Martin agar (TMA).
Results: The results showed that the mFB could inhibit the growth of E. coli, L. monocytogenes, S. agalactiae, and S. saprophyticus but did not affect the growth of N. gonorrhoeae and significantly enhanced its growth. Using mFB, N. gonorrhoeae recovered 100% (8/8) of the positive Gram stain results from 77 clinical specimens, while direct TMA culture only recovered 75% (6/8). In addition, mFB enabled the detection of N. gonorrhoeae in 2 of the 69 Gram stain-negative specimens that were negative by direct TMA culture.
Conclusion: N. gonorrhoeae culture using mFB, followed by subculture on CA, indicated that the mFB can preserve N. gonorrhoeae in clinical specimens during delivery to the laboratory and promote its growth. This has the potential to improve gonorrhea diagnosis and treatment with appropriate antibiotics, as well as enhance surveillance of antimicrobial-resistant gonorrhea.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Lin EY, Adamson PC, Klausner JD. Epidemiology, Treatments, and Vaccine Development for AntimicrobialResistant Neisseria gonorrhoeae: Current Strategies and Future Directions. Drugs. 2021; 81(10): 1153-69.
World Health Organization. Report on global sexually transmitted infection surveillance 2018.
Keshvani N, Gupta A, Incze MA. I am worried about gonorrhea: what do i need to know? JAMA Intern Med.2019; 179(1): 132. doi.org/10.1001/jamaintern med.2018.4345.
Fingerhuth SM, Bonhoeffer S, Low N, Althaus CL. Antibiotic-Resistant Neisseria gonorrhoeae Spread Faster with More Treatment, Not More Sexual Partners. PLoS Pathog. 2016; 12: 1-15. doi.org/ 10.1371/journal.ppat.1005611, PMID: 27196299
Unemo M, Lahra MM, Cole M, Galarza P, Ndowa F, Martin I, et al. World Health Organization Global Gonococcal Antimicrobial Surveillance Program (WHO GASP): review of new data and evidence to inform international collaborative actions and research efforts. Sex Health. 2019; 16(5): 412-25.
Unemo M, Golparian D, Eyre DW. Antimicrobial Resistance in Neisseria gonorrhoeae and Treatment of Gonorrhea. Methods Mol Biol. 2019; 1997: 37-58. doi: 10.1007/978-1-4939-9496-0_3. PMID: 31119616.
Pleininger S, Indra A, Golparian D, Heger F, Schindler S, Jacobsson S, et al. Extensively drug-resistant (XDR) Neisseria gonorrhoeae causing possible gonorrhoea treatment failure with ceftriaxone plus azithromycin in Austria, April 2022. Euro Surveill. 2022; 27(24): 2200455. doi: 10.2807/1560-7917.ES.2022.27.24.220045
Kittiyaowamarn R, Girdthep N, Cherdtrakulkiat T, Sangprasert P, Tongtoyai J, Weston E, et al. Neisseria gonorrhoeae antimicrobial susceptibility trends in Bangkok, Thailand, 2015-21: Enhanced Gonococcal Antimicrobial Surveillance Programme (EGASP). JAC Antimicrob Resist. 2023; (6): dlad139. doi: 10.1093/ jacamr/dlad139.
Ison CA, Golparian D, Saunders P, Chisholm S, Unemo M. Evolution of Neisseria gonorrhoeae is a continuing challenge for molecular detection of gonorrhoea: False negative gonococcal porA mutants are spreading internationally. Sex Transm Infect. 2013; 89: 197-201. doi.org/10.1136/sextrans-2012-050829 PMID: 23241969
Murray PR, Baron EJ, Pfaller MA, Tenover FC, Yolken RH editors. Manual of Clinical Microbiology 7th Ed. Washington, DC: ASM Press; 1999. p.64-104: 777-806.
Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing, 32nd Ed. CLSI supplement M100 (ISBN 978- 1-68440-134-5 [Print]; ISBN 978-1-68440-135-2 [Electronic]). Clinical and Laboratory Standards Institute, USA, 2022.
Cartwright CP, Stock F, Gill VJ. Improved enrichment broth for cultivation of fastidious organisms. J Clin Microbiol. 1994; 32(7): 1825-6. doi: 10.1128/jcm.32. 7.1825-1826.1994.
Kazemi Rad S, Assmar M, Mirpour M, Razavi MR Evaluation of Chitosan Nanoparticle Antimicrobial Effect on Isolated Listeria monocytogenes Bacteria from Pregnant Women and L. monocytogenes ATCC 7644 Iran J Public Health 2022; 51(12): 2783-90. doi: 1018502/ijphv51i1211469 PMID: 36742246; PMCID: PMC9874196.
Khademi F, Sahebkar A Group B streptococcus drug resistance in pregnant women in Iran: a metaanalysis Taiwan J Obstet Gynecol 2020; 59(5): 635-42 doi: 101016/jtjog202007002 PMID: 32917310.
Zhou Y, Zhou Z, Zheng L, Gong Z, Li Y, Jin Y, et al. Urinary Tract Infections Caused by Uropathogenic Escherichia coli: Mechanisms of Infection and Treatment Options. Int J Mol Sci. 2023; 24(13): 10537. doi: 10.3390/ijms241310537.
Thayer JD, Martin JE Jr. Improved medium selective for cultivation of N. gonorrhoeae and N. meningitidis. Public Health Rep (1896). 1966; 81(6): 559-62. PMID: 4957043; PMCID: PMC1919807.
Unemo M, Shafer WM. Antimicrobial Resistance in Neisseria gonorrhoeae in the 21st Century: Past, Evolution, and Future. Clin Microbio Rev. 2014; 27(3):587-613. doi: 10.1128/CMR.00010-14
Samuel LP, Balada-Llasat JM, Harrington A, Cavagnolo R. Multicenter Assessment of Gram Stain Error Rates. J Clin Microbiol. 2016; 54(6): 1442-7. doi: 10.1128/ JCM.03066-15 PMID: 26888900; PMCID: PMC4879281.