Preliminary study: Exploring the influence of healthcare services and antibiotic discontinuation among pulmonary tuberculosis patients with self-administration in Western Thailand: A case-control study
Main Article Content
Abstract
Background: Outpatients generally use self-administration, which might result in defaulting from treatment.
Objective: This study evaluated the association between patient treatment discontinuation and health service.
Materials and methods: This retrospective case-control study was conducted in a TB clinic at Makarak Hospital, Kanchanaburi Province, Thailand. Participants who completed and discontinued treatment from 2017 to 2021 were surveyed using questionnaires.
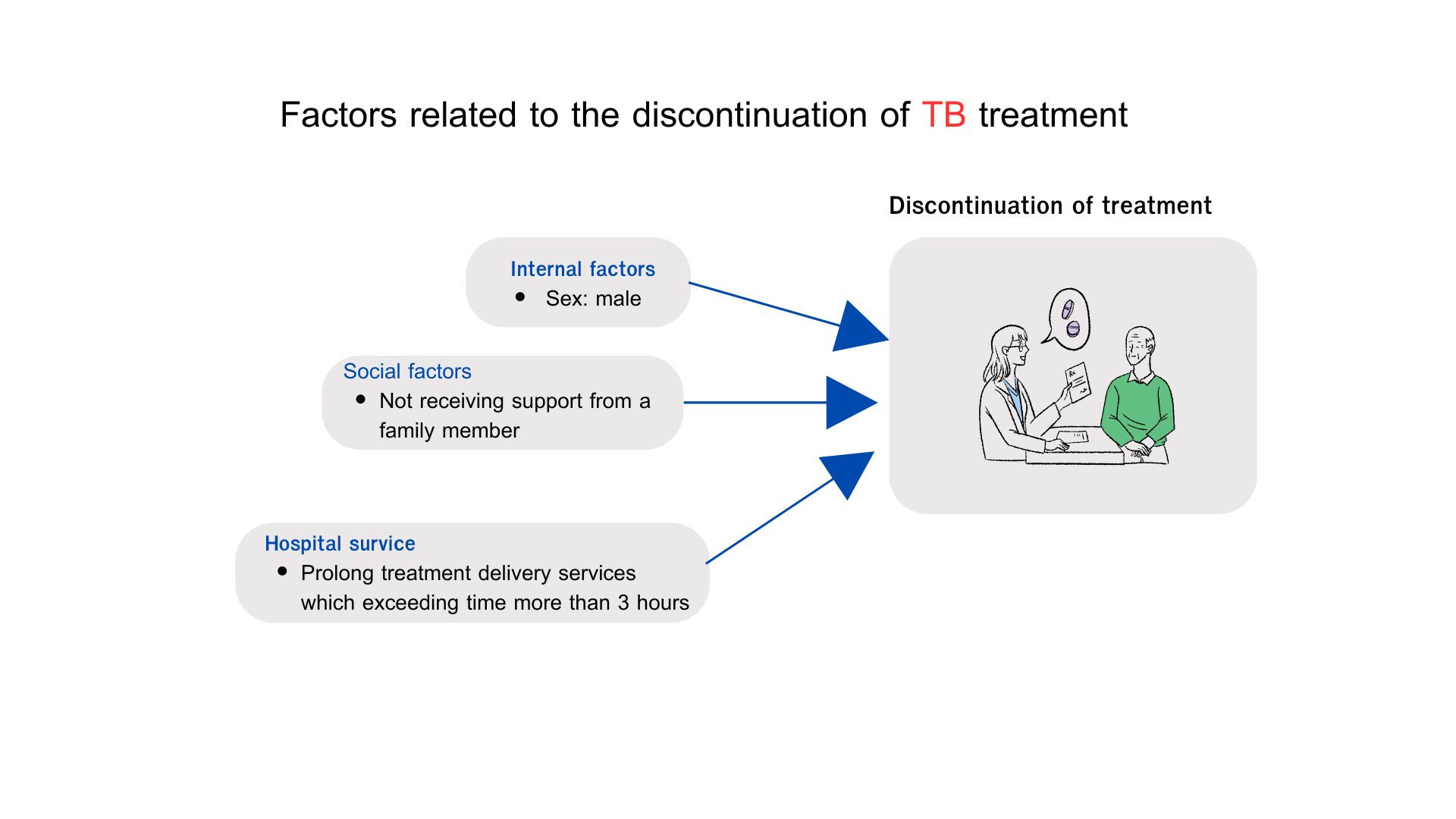
Results: A total of 198 patients with TB who discontinued (N=49) and completed treatment (N=149) were analyzed. Associated factors of discontinued treatment in those who were male were (OR=8.41, 95%CI: 1.55-45.61), not receiving support from a family member (OR=33.75, 95%CI: 3.22-353.76), and waiting time of more than 3 hours for health services (OR=9.39, 95%CI: 1.98-44.64).
Conclusion: Prolong treatment delivery services that exceed more than 3 hours and living without family support were associated with drug discontinuation in patients with TB who were self-administration treatment. These factors should be considered to enhance TB treatment success and infection control.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Salame FM, Ferreira MD, Belo MT, Teixeira EG, CordeiroSantos M, Ximenes RA, et al. Knowledge about tuberculosis transmission and prevention and perceptions of health service utilization among index cases and contacts in Brazil: Understanding losses in the latent tuberculosis cascade of care. Hasnain SE, editor. PLoS ONE. 2017; 12(9): e0184061. doi. org/10.1371/journal.pone.0184061.
WHO. Global tuberculosis report 2022 [Internet]. Geneva; 2022 [cited 2023 Oct 15]. Available from: https://www.who.int/teams/global-tuberculosisprogramme/tb-reports/global-tuberculosis-report-2022.
WHO. Global Tuberculosis Report 2023 [Internet]. 2023 [cited 2024 May 31]. Available from: https:// www.who.int/teams/global-tuberculosis-programme/ tb-reports/global-tuberculosis-report-2023.
Jiraphongsa C, Wangteeraprasert T, Henpraserttae N, Sanguanwongse N, Panya L, Sukkasitvanichkul J, et al. Community outbreak of multidrug resistance tuberculosis, Kanchanaburi province, Thailand on 2002- June 2010. J Prev Med Assoc Thai. 2011; 1: 261-71.
Sujariyakul A, Rudeeaneksin J, Tipkrua N, Phetsuksiri B. Epidemiology and genotypes of Mycobacterium tuberculosis at an outbreak area in Kanchanaburi province. Dis Control J. 2016; 42(4): 337-47. doi.org/10. 14456/dcj.2016.7.
Muture BN, Keraka MN, Kimuu PK, Kabiru EW, Ombeka VO, Oguya F. Factors associated with default from treatment among tuberculosis patients in nairobi province, Kenya: A case control study. BMC Public Health. 2011; 11(1): 696. doi.org/10.1186/1471-2458- 11-696.
Garrido M da S, Penna ML, Perez-Porcuna TM, Souza AB de, Marreiro L da S, Albuquerque BC, et al. Factors Associated with Tuberculosis Treatment Default in an Endemic Area of the Brazilian Amazon: A Case Control-Study. PLOS ONE. 2012; 7(6): e39134. doi. org/10.1371/journal.pone.0039134.
WHO. WHO consolidated guidelines on tuberculosis. Module 4: treatment - drug-resistant tuberculosis treatment, 2022 update. Geneva; 2022.
Tian JH, Lu ZX, Bachmann MO, Song FJ. Effectiveness of directly observed treatment of tuberculosis: a systematic review of controlled studies. Int J Tuberc Lung Dis. 2014; 18(9): 1092-8. doi.org/ 10.5588/ ijtld.13.0867.
Pasipanodya JG, Gumbo T. A meta-analysis of selfadministered vs directly observed therapy effect on microbiologic failure, relapse, and acquired drug resistance in tuberculosis patients. Clin Infect Dis. 2013; 57(1): 21-31. doi.org/ 10.1093/cid/cit167.
Namukwaya E, Nakwagala F, Mulekya F, MayanjaKizza H, Mugerwa R. Predictors of treatment failure among pulmonary tuberculosis patients in Mulago hospital, Uganda. Afr Health Sci. 2011; 11(Suppl 1): S105-11. doi.org/ 10.4314/ahs.v11i3.70079.
Zegeye A, Dessie G, Wagnew F, Gebrie A, Islam SMS, Tesfaye B, et al. Prevalence and determinants of antituberculosis treatment non-adherence in Ethiopia: A systematic review and meta-analysis. PLOS ONE. 2019; 14(1): e0210422. doi.org/ 10.1371/journal. pone.0210422.
Dodor EA, Afenyadu GY. Factors associated with tuberculosis treatment default and completion at the Effia-Nkwanta Regional Hospital in Ghana. Trans R Soc Trop Med Hyg. 2005; 99(11): 827-32. doi.org/ 10.1016/j.trstmh.2005.06.011.
Mekonnen HS, Azagew AW. Non-adherence to antituberculosis treatment, reasons and associated factors among TB patients attending at Gondar town health centers, Northwest Ethiopia. BMC Research Notes. 2018; 11(1): 691. doi.org/ 10.1186/s13104-018- 3789-4.
Gugssa Boru C, Shimels T, Bilal AI. Factors contributing to non-adherence with treatment among TB patients in Sodo Woreda, Gurage Zone, Southern Ethiopia: A qualitative study. Infect Public Health. 2017; 10(5): 527-33. doi.org/ 10.1016/j.jiph.2016.11.018.
Jiraphongsa C, Wangteeraprasert T, Henpraserttae N, Sanguanwongse N, Panya L, Sukkasitvanichkul J, et al. Community outbreak of multidrug resistance tuberculosis, Kanchanaburi province, Thailand on 2002-June 2010. J Prev Med Assoc Thail. 2011; 1: 261-71.
Sujariyakul A, Rudeeaneksin J, Tipkrua N, Phetsuksiri B. Epidemiology and genotypes of Mycobacterium tuberculosis at an outbreak area in Kanchanaburi province. Dis Control J. 2016 ; 42(4): 337-47.
Herrero MB, Ramos S, Arrossi S. Determinants of non adherence to tuberculosis treatment in Argentina: barriers related to access to treatment. Rev bras epidemiol. 2015; 18: 287-98. doi.org/ 10.1590/1980- 5497201500020001.
Umo I, Kulai M, Commons RJ. Factors associated with loss to follow-up among TB patients in rural Papua New Guinea. Public Health Action. 2021; 11(4): 186-90. doi.org/ 10.5588/pha.21.0054.
Slama K, Tachfouti N, Obtel M, Nejjari C. Factors associated with treatment default by tuberculosis patients in Fez, Morocco. East Mediterr Health J. 2013; 19(08): 687-93.
Suliman Q, Lim PY, Md. Said S, Tan KA, Mohd. Zulkefli NA. Risk factors for early TB treatment interruption among newly diagnosed patients in Malaysia. Sci Rep. 2022; 12(1): 745. doi.org/ 10.1038/s41598-021- 04742-2.
Gube AA, Debalkie M, Seid K, Bisete K, Mengesha A, Zeynu A, et al. Assessment of Anti-TB Drug Nonadherence and Associated Factors among TB Patients Attending TB Clinics in Arba Minch Governmental Health Institutions, Southern Ethiopia. Tuberc Res Treat. 2018; 2018: e3705812. doi.org/ 10.1155/2018/3705812.