Assessment of dose uniformity and optimal CT number for virtual bolus in breast VMAT planning
Main Article Content
Abstract
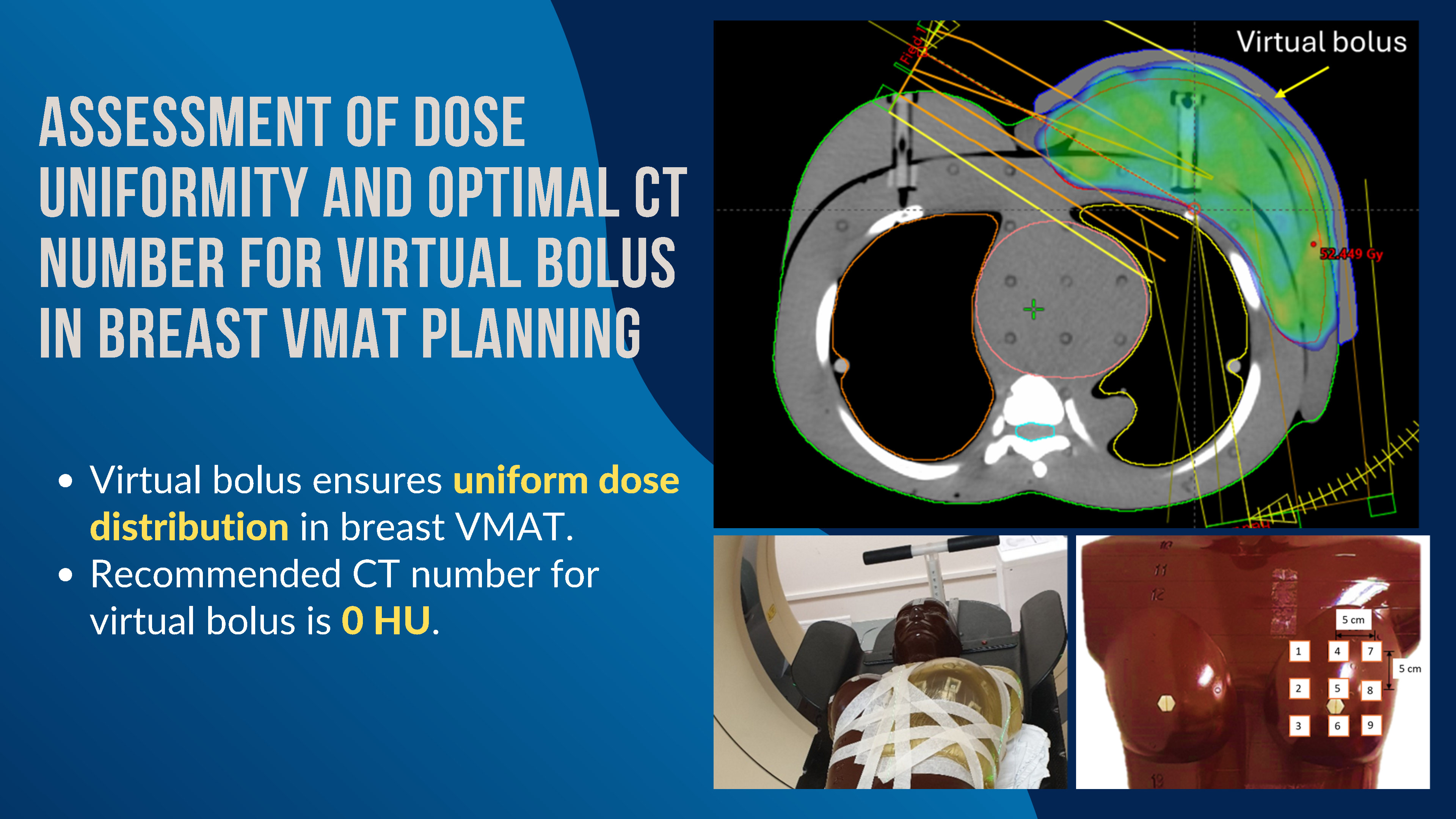
Background: ICRU Report No. 83 proposes using the Flash Region in the strategic design of breast cancer treatment. However, concerns persist regarding the delivery of the designated radiation dose to breast cancer patients undergoing Volumetric Modulated Arc Therapy (VMAT) with virtual bolus in the irradiation plan.
Objective: This study aimed to assess dose uniformity in breast VMAT treatment with a virtual bolus, validate the planning dose by comparing it with nanoDotTM measurements on a Rando phantom, and determine the optimal CT number for the virtual bolus in breast VMAT planning. Materials and
Materials and methods: To assess dose uniformity in the breast VMAT plan, nine nanoDot™ dosimeters were placed on the breast of Rando phantom, followed by CT simulation and VMAT treatment planning. The clinical target volume (CTV) and organs at risk were contoured, and the planning target volume (PTV) boundaries were expanded by 5 mm and 10 mm for virtual bolus thicknesses of 10 mm and 15 mm, respectively. The CT number of the virtual bolus varied from 0 to -700 HU. The planning doses at 9 points were determined, and the coefficient of variation (%CV) was calculated. Additionally, measurements at these 9 points were performed using nanoDot™ dosimeters. The calculated and measured doses were then compared. Finally, VMAT treatment plans with a virtual bolus were implemented in 10 breast cancer patients, using the virtual bolus with varying CT numbers as in the phantom study to evaluate the optimal CT number of the bolus.
Results: The doses among the 9 points for each plan were uniform, with a %CV of less than 4. For calculated dose validation, the percentage differences between the measured and calculated dose for all treatment plans, with variations in the CT number and the bolus thickness, were within ±5%. To determine the optimal CT number for the virtual bolus, the breast cancer treatment plan that met the dose criteria for tumors and organs at risk was the plan with a CT number of 0 HU for both virtual bolus thicknesses of 10 and 15 mm.
Conclusion: Virtual bolus provides uniform dose distribution for breast VMAT planning, which measurements from nanoDotTM can validate. The appropriate CT number for the virtual bolus is 0 HU for both bolus thicknesses. In future studies, measurements should be conducted on actual patients.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Lizondo M, Latorre-Musoll A, Ribas M, Carrasco P, Espinosa N, Coral A et al. Pseudo skin flash on VMAT in breast radiotherapy: Optimization of virtual bolus thickness and HU values. Physica Medica 2019; 63: 56-62. doi: 10.1016/j.ejmp.2019.05.010.
Monajemi TT, Oliver PAK, Day A, Yewondwossen M. In search of a one plan solution for VMAT postmastectomy chest wall irradiation. J Appl Clin Med Phys 2020; 21(8): 216-23. doi:10.1002/acm2.12948.
Bogue J, Wan J, Lavey RS, Parsai EI. Dosimetric comparison of VMAT with integrated skin flash to 3D field-in-field tangents for left breast irradiation. J Appl Clin Med Phys 2019; 20(2): 24-9. doi:10.1002/ acm2.12527.
ICRU. Prescribing, Recording, and Reporting PhotonBeam Intensity-Modulated Radiation Therapy (IMRT), ICRU Report 83. 2010. doi:10.1093/jicru/ndq010.
Rossi M, Boman E, Skyttä T, Haltamo M, Laaksomaa M, Kapanen M. Dosimetric effects of anatomical deformations and positioning errors in VMAT breast radiotherapy. J Appl Clin Med Phys 2018; 19(5): 506- 16. doi:10.1002/acm2.12409.
Tyran M, Tallet A, Resbeut M, Ferre M, Favrel V, Fau P et al. Safety and benefit of using a virtual bolus during treatment planning for breast cancer treated with arc therapy. J Appl Clin Med Phys 2018; 19(5): 463-72. doi:10.1002/acm2.12398.
Yukihara EG, Yoshimura EM, Lindstrom TD, Ahmad S, Taylor KK, Mardirossian G. High-precision dosimetry for radiotherapy using the optically stimulated luminescence technique and thin Al2O3:C dosimeters. Phys Med Biol 2005; 50(23): 5619-28. doi:10.1088/0031-9155/50/23/014.
Jursinic PA. Characterization of optically stimulated luminescent dosimeters, OSLDs, for clinical dosimetric measurements. Med Phys 2007; 34(12): 4594-604. doi:10.1118/1.2804555.
Dunn L, Lye J, Kenny J, Lehmann J, Williams I, Kron T. Commissioning of optically stimulated luminescence dosimeters for use in radiotherapy. Radiat Meas 2013; 51-2: 31–39. doi:10.1016/j.radmeas.2013.01.012.
Viamonte A, Da Rosa LAR, Buckley LA, Cherpak A, Cygler JE. Radiotherapy dosimetry using a commercial OSL system. Med Phys 2008; 35(4): 1261-6. doi:10.1118/1.2841940.
Alvarez P, Kry SF, Stingo F, Followill D. TLD and OSLD dosimetry systems for remote audits of radiotherapy external beam calibration. Radiat Meas 2017; 106: 412-5. doi:10.1016/j.radmeas.2017.01.005.
Mrčela I, Bokulić T, Izewska J, Budanec M, Fröbe A, Kusić Z. Optically stimulated luminescence in vivo dosimetry for radiotherapy: Physical characterization and clinical measurements in 60Co beams. Phys Med Biol 2011; 56(18): 6065-82. doi:10.1088/0031- 9155/56/18/018.
Yusof FH, Ung NM, Wong JHD, Jong WL, Ath V, Phua VCE et al. On the use of optically stimulated luminescent dosimeter for surface dose measurement during radiotherapy. PLoS One 2015; 10(6): 1-15. doi: 10.1371/journal.pone.0128544.
Zhuang AH, Olch AJ. Validation of OSLD and a treatment planning system for surface dose determination in IMRT treatments. Med Phys 2014; 41(8): 081720doi:10.1118/1.4890795.
Wake JR, Chen FQ, Ashworth S, Byth K, Wang W, Stuart KE. Verification using in vivo optically stimulated luminescent dosimetry of the predicted skin surface dose in patients receiving postmastectomy radiotherapy. Medical Dosimetry 2021; 46(2): e1-e6. doi:10.1016/j.meddos.2020.10.001.
Butson M, Chen T, Alzaidi S, Pope D, Butson E, Gorjiara T et al. Extrapolated skin dose assessment with optically stimulated luminescent dosimeters. Biomed Phys Eng Express 2016; 2(4): 47001. doi:10.1088/2057-1976/2/4/047001.
Raj LJS, Pearlin B, Peace BST, Isiah R, Singh IRR. Characterisation and use of OSLD for in vivo dosimetry in head and neck intensity-modulated radiation therapy. J Radiother Pract 2021; 20(4): 448- 54. doi:10.1017/S146039692000062X.
Ponmalar R, Manickam R, Ganesh KM, Saminathan S, Raman A, Godson HF. Dosimetric characterization of optically stimulated luminescence dosimeter with therapeutic photon beams for use in clinical radiotherapy measurements. J Cancer Res Ther 2017; 13(2): 304-12. doi:10.4103/0973-1482.199432.
IAEA. Absorbed Dose Determination in External Beam Radiotherapy, Technical Reports Series No. 398 (Rev. 1). INTERNATIONAL ATOMIC ENERGY AGENCY: Vienna, 2024; doi:10.61092/iaea.ve7q-y94k.
Feuvret L, Noël G, Mazeron JJ, Bey P. Conformity index: A review. Int J Radiat Oncol Biol Phys 2006; 64(2): 333-42. doi:10.1016/j.ijrobp.2005.09.028.
Freedman GM, White JR, Rosenstein B, Bentzen SM, Li A, Co-Chair S et al. Radiation therapy oncology group RTOG 1005 a phase III trial of accelerated whole breast irradiation with hypofractionation plus concurrent boost versus standard whole breast irradiation plus sequential boost for early-stage breast cancer, Study Chairs Document History. 2011 [cited 2024 May 14]. Available from: https://www. ctsu.org.
IAEA. Development of Procedures for In Vivo Dosimetry in Radiotherapy, IAEA HUMAN HEALTH REPORTS No. 8. 2013 [cited 2024 May 14]. Available from: https://www-pub.iaea.org/MTCD/publications/PDF/ Pub1606_web.pdf.
Kerns JR, Kry SF, Sahoo N, Followill DS, Ibbott GS. Angular dependence of the nanoDot OSL dosimeter. Med Phys 2011; 38(7): 3955-62. doi:10. 1118/1.3596533.
Frazier RC, Vicini FA, Sharpe MB, Yan D, Fayad J, Baglan KL et al. Impact of breathing motion on whole breast radiotherapy: A dosimetric analysis using active breathing control. Int J Radiat Oncol Biol Phys 2004; 58(4): 1041-7. doi:10.1016/j.ijrobp.2003.07.005.