Effect of postural breath technique (PBT) compared with postural stretching technique (PST) on body flexibility in healthy participants with poor flexibility: A randomized controlled trial
Main Article Content
Abstract
Background: Body flexibility is essential in sports science, enhancing athletic performance by improving agility, balance, and coordination. Postural muscles serve postural control and breathing and are crucial in biomechanics and neurophysiology. The postural breath technique, an exercise combining breathing and postural muscle engagement, was designed to enhance flexibility.
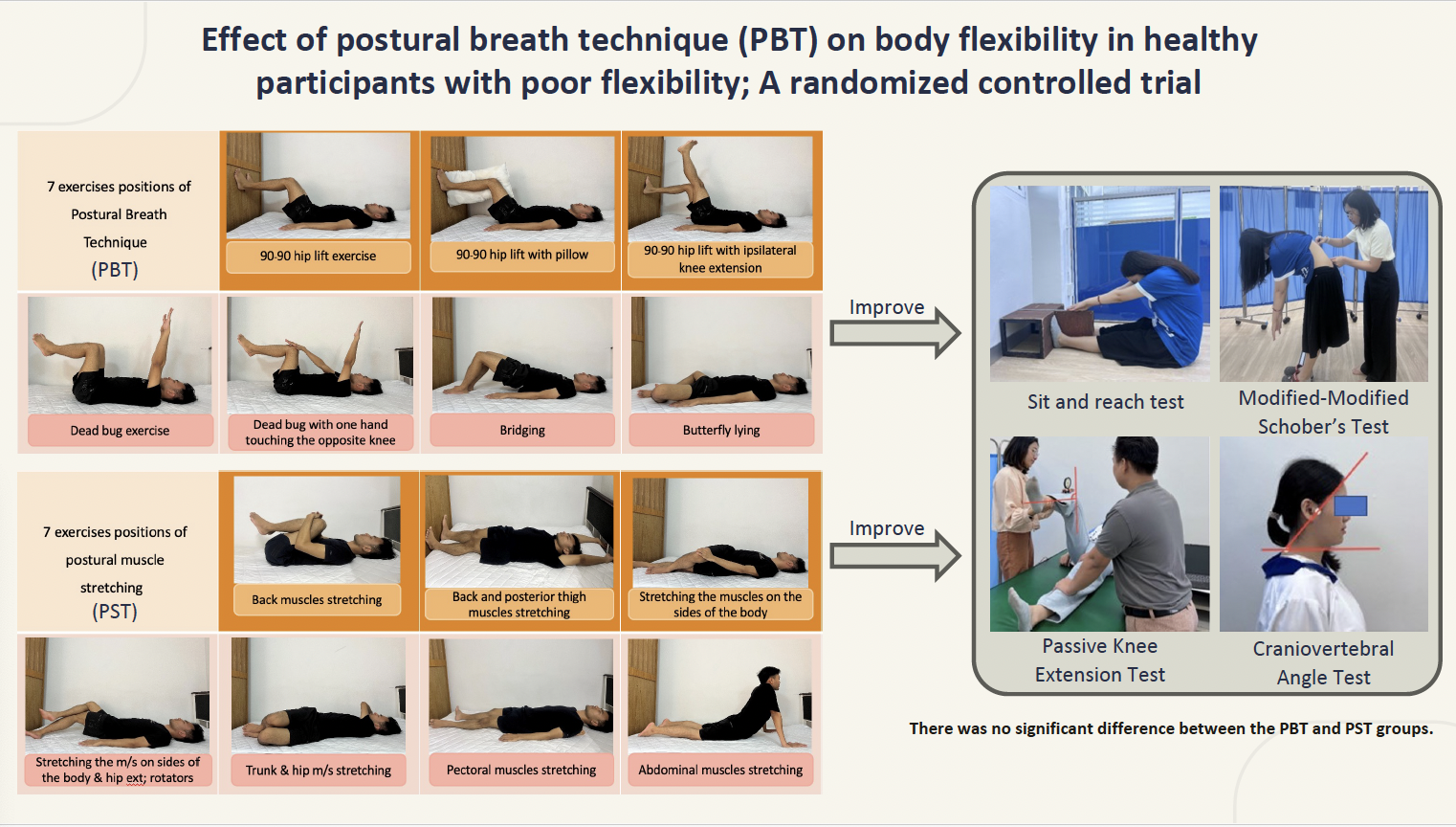
Objective: This study compared the effects of postural breath technique (PBT) and postural stretching technique (PST) on body flexibility in individuals with poor flexibility.
Materials and methods: Fifty-eight participants with poor flexibility were randomly divided into two groups. They received a supervised exercise program of either PBT or PST twice weekly for four weeks. Outcome measurements, including Sit and Reach Test (SRT) as the primary outcome, Modified-modified Schober Test (MMST), Passive Knee Extension Test (PKE), and Craniovertebral Angle Test (CVA) as secondary outcomes, were conducted at baseline, immediately after the first session, and after the last session.
Results: Within each group, both PBT and PST significantly increased SRT scores, decreased PKE angle on both sides and improved MMST and CVA. The mixed-model ANOVA revealed significant differences within groups at each assessment point. PBT resulted in immediate and after four weeks improvements in SRT, MMST, PKE, and CVA, while PST showed increased of all outcomes after four weeks. However, there was no significant difference between the PBT and PST groups.
Conclusion: Both PBT and PST demonstrated effectiveness in improving general body and hamstring flexibility. The study’s results suggest that clinicians determine the most effective approach for everyone, such as immediate flexibility improvements (PBT) or sustained flexibility gains over time (PST).
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Pfeifer CE, Ross LM, Weber SR, Sui X, Blair SN. Are flexibility and muscle-strengthening activities associated with functional limitation? Sports Med Health Sci. 2022; 4(2): 95-100. doi: 10.1016/j.smhs.2022.03.001.
Mocanu GD, Dobrescu T. Improving upper body flexibility in students through various types of stretching during physical education lessons. J Phys Educ Sport. 2021; 21(3): 1533-43. doi: 10.7752/jpes.2021.03195.
Raftry SM, Marshall PWM. Does a ‘tight’ hamstring predict low back pain reporting during prolonged standing? J Electromyogr Kinesiol. 2012; 22(3): 407-11. doi: 10.1016/j.jelekin.2012.02.008.
Reis FJ, Macedo AR. Influence of hamstring tightness in pelvic, lumbar and trunk range of motion in low back pain and asymptomatic volunteers during forward bending. Asian Spine J. 2015; 9(4): 535-40. doi: 10.4184/asj.2015.9.4.535.
Lee K. The relationship of trunk muscle activation and core stability: a biomechanical analysis of pilates-based stabilization exercise. Int J Environ Res Public Health. 2021; 18(12804): 1-11. doi: 10.3390/ijerph182312804.
Srijessadarak T, Arayawichanon P, Kanpittaya J, Boonprakob Y. Diaphragmatic Mobility and Chest Expansion in Patients with Scapulocostal Syndrome: A Cross-Sectional Study. Healthcare. 2022; 10(950): 1-9. doi: 10.3390/healthcare10050950.
Shankar G, Chaurasia V. Comparative study of core stability exercise with Swiss ball in improving trunk endurance. Int J Health Sci Res. 2012; 2(5): 57-61.
Swann J. Good positioning: the importance of posture. NRC. 2009; 11(9): 467-9. doi: 10.12968/nrec.2009.11.9.43734.
Kocjan J, Gzik-Zroska B, Nowakowska K, Burkacki M, Suchoń S, Michnik R, et al. Impact of diaphragm function parameters on balance maintenance. PLoS One. 2018; 13(12): 1-14. doi: 10.1371/journal.pone.0208697.
Magee D. Thoracic (dorsal) spine, Lumbar spine. Orthopedic Physical Assessment, 6th Ed., Elsevier: Amsterdam, The Netherlands, 2013, 508-648.
Tomaszewska A, Pawlicka-Lisowska A. Evaluation of an influence of systematic motor activity on the body posture of young people. Pol Merkur Lek. 2014; 36(215): 336-40.
Csepregi É, Gyurcsik Z, Veres-Balajti I, Nagy AC, Szekanecz Z, Szántó S. Effects of classical breathing exercises on posture, spinal and chest mobility among female university students compared to currently popular training programs. Int J Environ Res Public Health. 2022; 19(3728): 1-22. doi: 10.3390/ijerph19063728.
Granacher U, Schellbach J, Klein K, Prieske O, Baeyens JP, Muehlbauer T. Effects of core strength training using stable versus unstable surfaces on physical fitness in adolescents: a randomized controlled trial. BMC Sports Sci Med Rehabil. 2014; 6(1): 1-11. doi: 10.1186/2052-1847-6-40.
Kalaycioglu T, Apostolopoulos NC, Goldere S, Duger T, Baltaci G. Effect of a core stabilization training program on performance of ballet and modern dancers. J Strength Cond Res. 2020; 34(4): 1166-75. doi: 10.1519/JSC.0000000000002916.
Hruska R, Coughlin KJ, Masek J. Cough-variant asthma: Responsive to integrative management and postural restoration. Explore. 2005; 1(5): 377-9. doi: 10.1016/j.explore.2005.06.008.
Batista LH, Vilar AC, de Almeida Ferreira JJ, Rebelatto JR, Salvini TF. Active stretching improves flexibility, joint torque, and functional mobility in older women. Am J Phys Med Rehabil. 2009; 88(10): 815-22. doi: 10.1097/PHM.0b013e3181b72149.
Phrompaet S, Paungmali A, Pirunsan U, Sitilertpisan P. Effects of pilates training on lumbo-pelvic stability and flexibility. Asian J Sports Med. 2011; 2(1): 16-22. doi: 10.5812/asjsm.34822.
Charoenwipas P, Buabucha P, Arayawichanon P, Hansawong T, Matho L, Puangmali A, et al. Therapeutic effects of posture breath technique in patients with scapulocostal syndrome. Thai J Phys Ther. 2023; 45(1): 66-81 (in Thai).
Yıldırım MŞ, Tuna F, Demirbağ Kabayel D, Süt N. The cut-off values for the diagnosis of hamstring shortness and related factors. Balk Med J. 2018; 35(5): 388-93. doi: 10.4274/balkanmedj.2017.1517.
Joshi DG, Balthillaya G, Prabhu A. Effect of remote myofascial release on hamstring flexibility in asymptomatic individuals - A randomized clinical trial. J Bodyw Mov Ther. 2018; 22(3): 832-7. doi: 10.1016/j.jbmt.2018.01.008.
Na’ima AL, Sari GM, Utomo DN. Combination effect of core stability exercise and contract relax exercise on hamstring flexibility. J Phys Conf Ser. 2019; 1146(012035): 1-5. doi: 10.1088/1742-6596/1146/1/012035.
Frison L, Pockok SJ. Repeated measures in clinical trials: analysis using mean summary statistics and its implication for design. Statist Med. 1992; 11(13): 1685-704.
Ayala F, de Baranda PS, Croix MD, Santonja F. Reproducibility and criterion-related validity of the sit and reach test and toe touch test for estimating hamstring flexibility in recreationally active young adults. Phys Ther Sport. 2012; 13(4): 219-26. doi: 10.1016/j.ptsp.2011.11.001.
Rezvani A, Ergin O, Karacan I, Oncu M. Validity and reliability of the metric measurements in the assessment of lumbar spine motion in patients with ankylosing spondylitis. Spine. 2012; 37(19): 1189-96. doi: 10.1097/BRS.0b013e31825ef954.
Liu H, Shen Y, Xiong Y, Zhou H, Mao Y, Shen Q, Hong W, et al. Psychometric properties of four common clinical tests for assessing hamstring flexibility in young adults. Front Physiol. 2022; 13(911240): 1-8. doi: 10.3389/fphys.2022.911240.
Gadotti IC, Armijo-Olivo S, Silveira A, Magee D. Reliability of the cranio-cervical posture assessment: visual and angular measurements using photographs and radiographs. J Manipulative Physiol Ther. 2013; 36(9): 619-25. doi: 10.1016/j.jmpt.2013.09.002.
McArdle WD, Katch FI, Katch VL. Exercise Physiology: Energy, Nutrition, and Human Performance. 6th Ed. Philadelphia: Lippincott Williams & Wilkins; 2007.
Shrier I, Gossal K. Myths and truths of stretching: individualized recommendations for healthy muscles. Phys Sportsmed. 2000; 28(8): 57-63. doi: 10.3810/psm.2000.08.1159.
Kubo K, Kanehisa H, Fukunaga T. Effect of stretching training on the viscoelastic properties of human tendon structures in vivo. J Appl Physiol. 2002; 92(2): 595-601. doi: 10.1152/japplphysiol.00658.2001.
Simons DG, Travell JG, Simons LS. Myofascial Pain and Dysfunction: The Trigger Point Manual. Volume 1, 2nd Ed. Baltimore: Williams & Wilkins; 1999.
Boonprakob Y, Phadungkit S, Nongharnpitak S, Srijessadarak T, Supasatean W, Nakhengrit C. Trigger point: Curable or palliative symptoms. Bull Chiang Mai Assoc Med Sci. 2016; 49(1): 155-66 (in Thai).
Liemohn W. Exercise Prescription and the Back. New York: McGraw-Hill; 2001.
Atilgan E, Tarakci D, Mutluay F. Examining the postural awareness and flexibility changes in physical therapy students who took clinical pilates class. Pak J Med Sci. 2017; 33(3): 640-4. doi: 10.12669/pjms.333.12808.
Brumitt J, Matheson JW, Meira EP. Core stabilization exercise prescription, part I: current concepts in assessment and intervention. Sports Health. 2013; 5(6): 504-9. doi: 10.1177/1941738113502451.
Byung-Sun Kong, Beom-Cheol Jeong, Kyung-Tae Yoo. Effect of breathing exercises via joint mobilization on the lung function and spinal alignment of straight-necked women. J Korean Soc Phys Med. 2020; 15(4): 55-65. doi: 10.13066/kspm.2020.15.4.55.
Hyong IH, Kang JH. The immediate effects of passive hamstring stretching exercises on the cervical spine range of motion and balance. J Phys Ther Sci. 2013; 25(1): 113-6. doi: 10.1589/jpts.25.113.
Khunkitti C, Mato L, Hunsawong T, Paungmali A, Boonprakob Y. Effects of occipito-frontal release with dorsiflexion technique (OFRDF) for improvement of superficial back line flexibility. J Assoc Med Sci. 2020; 54(1): 26-34. doi: 10.14456/jams.2021.4.
Bentivoglio M, Cotrufo T, Ferrari S, Tesoriero C, Mariotto S, Bertini G, Berzero A, Mazzarello P. The original histological slides of Camillo Golgi and his discoveries on neuronal structure. Front Neuroanat. 2019; 13:3. doi: 10.3389/fnana.2019.00003.
Aramaki Y. Relationship between postural control and respiratory movement during one-leg standing in healthy males. J Phys Ther Sci. 2023; 35(6): 479-82. doi: 10.1589/jpts.35.479.