The development of a cylindrical phantom for nanoDotTM calibration with multiple beam angles
Main Article Content
Abstract
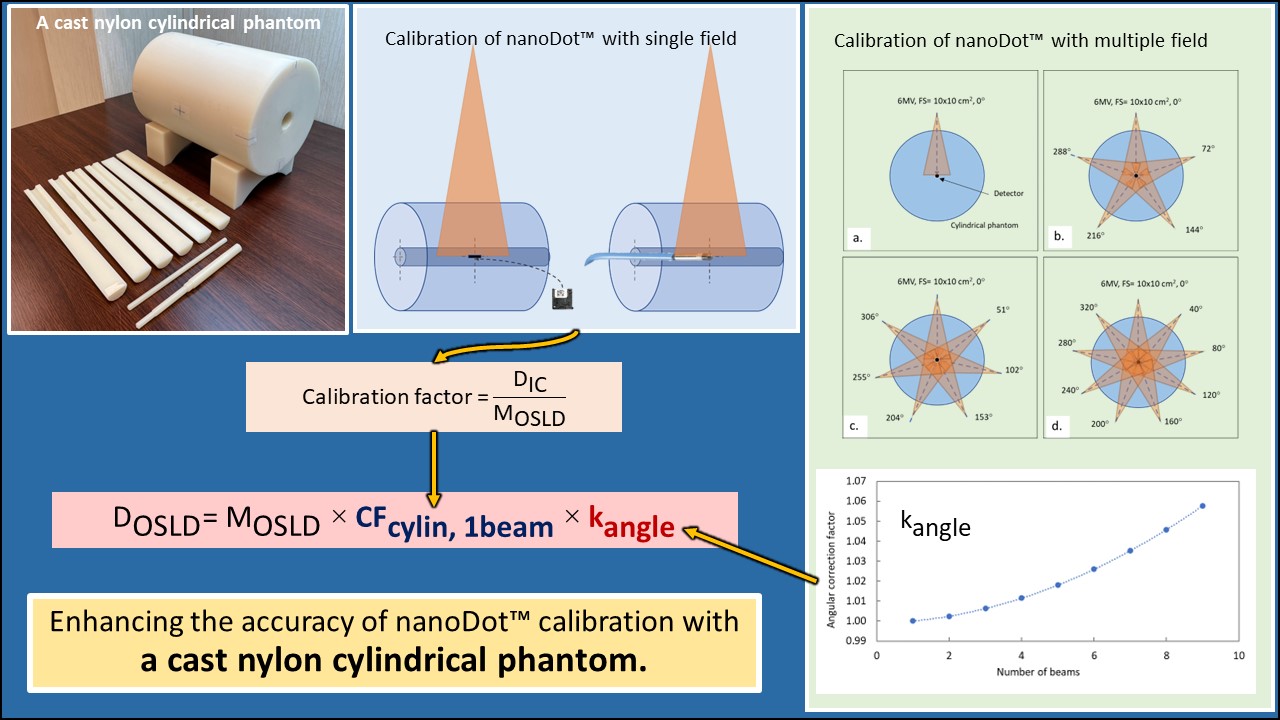
Background: The nanoDotTM dosimeter, an optically stimulated luminescent dosimeter (OSLD), is compact and precise, ideal for various applications like radiation dosimetry. The nanoDotTM requires calibration before use with the detector alignment perpendicular to the central beam axis. It exhibits angular dependence that may impact the calibration factor, requiring the fabrication of a specific cylindrical phantom for the calibration procedure.
Objective: This study aimed to develop a cylindrical phantom for nanoDotTM calibration to facilitate dose measurements in composite fields with various beam angles and to evaluate the nanoDotTM calibration factors for different plans.
Materials and methods: The cylindrical phantom was constructed using cast nylon material to accommodate the nanoDotTM or a cylindrical ionization chamber (IC). The novel phantom underwent validation for physical characteristics, including dimensions, density, and uniformity. Validation for the calibration factor, using cylindrical phantom (CF cylin) under standard conditions with a 10x10 cm² field size at 10 cm depth was conducted with 6 MV X-rays, comparing it with calibration factor using slab solid water phantoms (CFsolid). The CFcylin for different numbers of beams were determined and validated against a reference IC in various planning conditions. Furthermore, angular correction factors were determined for their application in the single-beam calibration factor.
Results: The cylindrical phantom had dimensions of 20 cm in diameter and 30 cm in length, a density of 1.145 g/cm³ and good uniformity. As a result of single beam, the CF cylin, agreed well with CFsolid, showing a difference of -0.069%. The CFcylin increased with the number of beams, ranging between 1.179 and 1.242. Additionally, the angular correction factor increased as the number of beams increased, peaking at 1.058 with 9 beams. When comparing the results to the IC, it was observed that with an increase in the number of beams to 4 beams, the single-beam calibration factor exhibited a variation of more than 2%. However, when applying the CF cylin specific to the number of beams or correcting for the angular correction factor, the dose differences between nanoDotTM and IC measurements were within 2%.
Conclusion: The developed cylindrical phantom is suitable for nanoDotTM calibration under single beam angle and in composite fields with various beam angles. The new calibration factors for specific numbers of beams allow for accurate dose measurements using nanoDotTM, thus reducing the dose difference from the IC to acceptable levels. Further studies should investigate its application in clinical situations.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Yukihara EG, Yoshimura EM, Lindstrom TD, Ahmad S, Taylor KK, Mardirossian G. High-precision dosimetry for radiotherapy using the optically stimulated luminescence technique and thin Al2O3:C dosimeters. Phys Med Biol [Internet]. 2005; 50(23): 5619-28. doi.org/10.1088/0031-9155/50/23/014.
Jursinic PA. Characterization of optically stimulated luminescent dosimeters, OSLDs, for clinical dosimetric measurements. Med Phys. 2007; 34(12): 4594-604. doi: 10.1118/1.2804555
Dunn L, Lye J, Kenny J, Lehmann J, Williams I, Kron T. Commissioning of optically stimulated luminescence dosimeters for use in radiotherapy. Radiat Meas. 2013; 51-52: 31-9. doi: 10.1016/j.radmeas.2013.01.012.
Viamonte A, Da Rosa LAR, Buckley LA, Cherpak A, Cygler JE. Radiotherapy dosimetry using a commercial OSL system. Med Phys. 2008; 35(4): 1261-6. doi: 10.1118/1.2841940.
Alvarez P, Kry SF, Stingo F, Followill D. TLD and OSLD dosimetry systems for remote audits of radiotherapy external beam calibration. Radiat Meas [Internet]. 2017; 106: 412-5. doi.org/10.1016/j.radmeas.2017.01.005.
Mrčela I, Bokulić T, Izewska J, Budanec M, Fröbe A, Kusić Z. Optically stimulated luminescence in vivo dosimetry for radiotherapy: Physical characterization and clinical measurements in 60Co beams. Phys Med Biol. 2011; 56(18): 6065-82. doi: 10.1088/0031-9155/56/18/018.
Yusof FH, Ung NM, Wong JHD, Jong WL, Ath V, Phua VCE, et al. On the use of optically stimulated luminescent dosimeter for surface dose measurement during radiotherapy. PLoS One. 2015; 10(6): 1-15. doi: 10.1371/journal.pone.0128544.
Zhuang AH, Olch AJ. Validation of OSLD and a treatment planning system for surface dose determination in IMRT treatments. Med Phys. 2014; 41(8): 081720. doi: 10.1118/1.4890795.
Wake JR, Chen FQ, Ashworth S, Byth K, Wang W, Stuart KE. Verification using in vivo optically stimulated luminescent dosimetry of the predicted skin surface dose in patients receiving postmastectomy radiotherapy. Med Dosim. 2021; 46(2): e1-6. doi: 10.1016/j.meddos.2020.10.001.
Butson M, Chen T, Alzaidi S, Pope D, Butson E, Gorjiara T, et al. Extrapolated skin dose assessment with optically stimulated luminescent dosimeters. Biomed Phys Eng Express. 2016; 2(4): 047001. doi: 10.1088/2057-1976/2/4/047001.
Raj LJS, Pearlin B, Peace BST, Isiah R, Singh IRR. Characterisation and use of OSLD for in vivo dosimetry in head and neck intensity-modulated radiation therapy. J Radiother Pract. 2021; 20(4): 448-54. doi: 10.1017/S146039692000062X.
Ponmalar R, Manickam R, Ganesh KM, Saminathan S, Raman A, Godson HF. Dosimetric characterization of optically stimulated luminescence dosimeter with therapeutic photon beams for use in clinical radiotherapy measurements. J Cancer Res Ther. 2017; 13(2): 304-12. doi: 10.4103/0973-1482.199432.
Kry SF, Alvarez P, Cygler JE, DeWerd LA, Howell RM, Meeks S, et al. AAPM TG 191: Clinical use of luminescent dosimeters: TLDs and OSLDs. Med Phys. 2020; 47(2): e19-51. doi: 10.1002/mp.13839.
Kerns JR, Kry SF, Sahoo N, Followill DS, Ibbott GS. Angular dependence of the nanoDot OSL dosimeter. Med Phys. 2011; 38(7): 3955-62. doi: 10.1118/1.3596533.
Yabung K, Khunnarong P, Wongsurija S. The application of OSLD for in vivo dosimetry in head and neck intensity-modulated radiation therapy: A phantom study [Thesis]. Faculty of Allied Health Sciences: Naresuan University; 2022 [in Thai].
Sookpeng S, Cheebsumon P, Pengpan T, Martin C. Comparison of computed tomography dose index in polymethyl methacrylate and nylon dosimetry phantoms. J Med Phys. 2016; 41(1): 45-51. doi: 10.4103/0971-6203.177287.
International Atomic Energy Agency. Quality Assurance for Computed Tomography - Diagnostic and Therapy Applications [HHS No.19]. Vienna: IAEA; 2012.
International Atomic Energy Agency. Absorbed Dose Determination in External Beam Radiotherapy [TRS398]. Vienna: IAEA; 2001.
International Atomic Energy Agency. Commissioning and Quality Assurance of Computerized Planning Systems for Radiation Treatment of Cancer (TRS 430). Vienna: IAEA; 2004.
International Atomic Energy Agency. Dosimetry of Small Static Fields used in External Beam Radiotherapy: An IAEA–AAPM International Code of Practice for Reference and Relative Dose Determination [TRS 483]. Vienna: IAEA; 2017.
Intang A, Oonsiri P, Kingkaew S, Chatchumnan N, Oonsiri S. Validation of the fabricated cast nylon head phantom for stereotactic radiosurgery end-toend test using alanine dosimeter. J Med Phys. 2023; 48(1): 74-9. doi: 10.4103/jmp.jmp_98_22.