Prevalence and associated factors of dyslipidemia among university students in Central Thailand: a cross-sectional study
Main Article Content
Abstract
Background: Dyslipidemia is regarded as a significant risk factor for atherosclerotic cardiovascular diseases (ASCVDs). Currently, there is limited data regarding dyslipidemia among Thai university students.
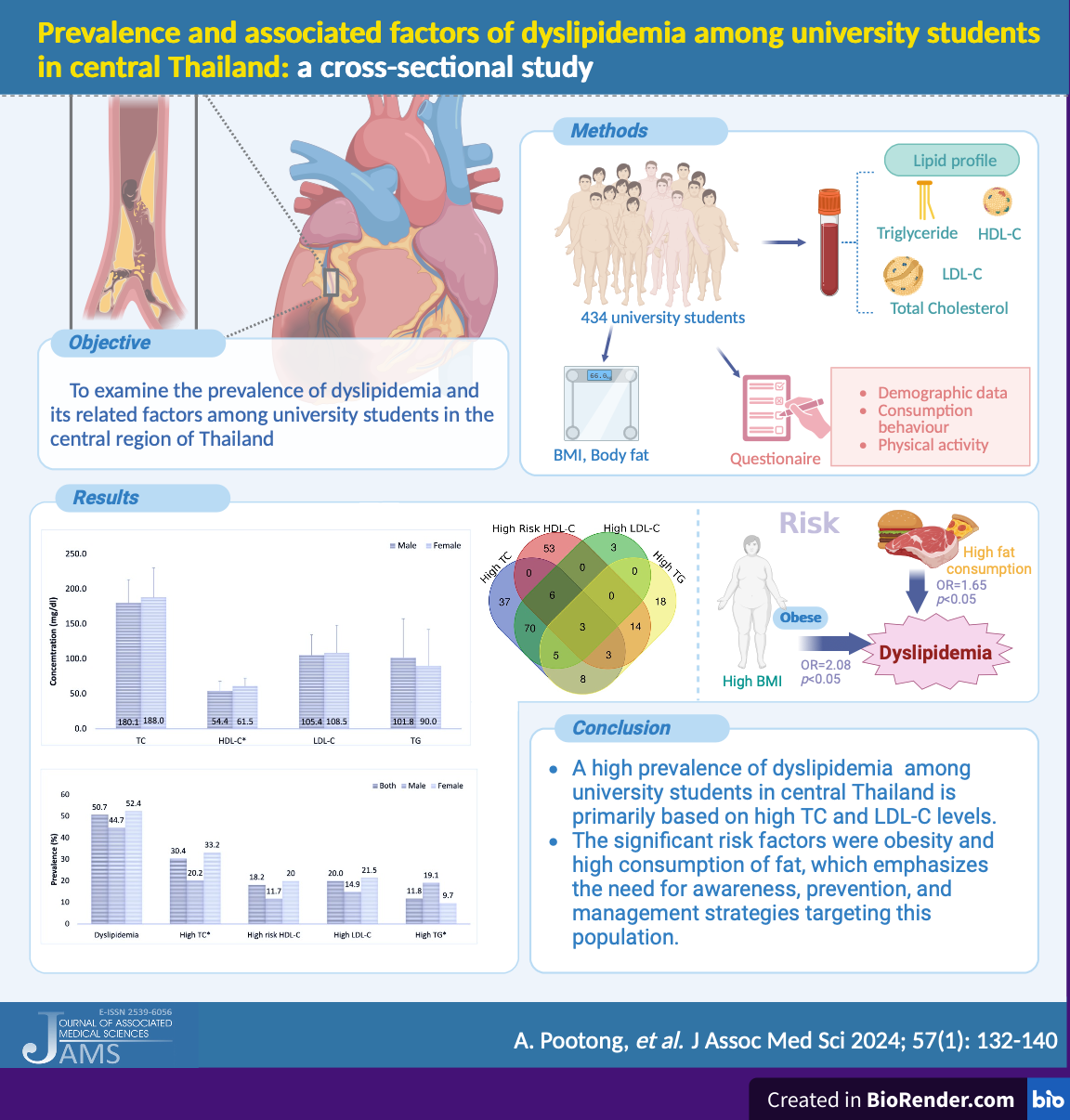
Objective: This study aimed to examine the prevalence of dyslipidemia and its related factors among university students in the central region of Thailand.
Materials and methods: In this cross-sectional study, a total of 434 students aged 18-25 years at Thammasat University and Kasetsart University were recruited using simple random sampling. Fasting venous blood samples were obtained, and plasma lipid profiles were assessed by an automated analyzer. Dyslipidemia was formally characterized according to the National Cholesterol Education Program Adult Treatment Panel (NCEP-ATP III) guidelines. Demographic information, dietary behavior, and physical activity were collected using questionnaires. Anthropometric measures were also performed according to a standard protocol.
Results: The prevalence of elevated total cholesterol, high-risk HDL-C, elevated LDL-C, and elevated triglycerides was 30.4, 18.2, 20.0, and 11.8%, respectively. The most common adverse lipid parameter was total cholesterol in both genders. Obesity and high fat intake were significantly associated with dyslipidemia (p<0.05).
Conclusion: This research revealed a significant occurrence of dyslipidemia, primarily driven by elevated total cholesterol, among university students in Thailand. Obesity and high fat intake are significant risk contributors to dyslipidemia. These findings emphasize the need for awareness, prevention, and management strategies targeting this population.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Sandesara P.B., Virani S.S., Fazio S., Shapiro M.D. The forgotten lipids: triglycerides, remnant cholesterol, and atherosclerotic cardiovascular disease risk. Endocr Rev. 2019; 40: 537-57. doi: 10.1210/er.2018-00184.
Mozaffarian D, Benjamin EJ, et al. Heart disease and stroke statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016; 133(4): e38-e360. doi: 10.1161/CIR.0000000000000350.
World Health Organization Western Pacific Region. Cardiovascular diseases (CVDs). Geneva: World Health Organization; 2021. [cited 2023 Sep 7]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Al-Duais MA, Al-Awthan YS. Prevalence of dyslipidemia among students of a Yemeni University. J Taibah Univ Med Sci. 2019; 14(2): 163-71. doi: 10.1016/j.jtumed.2018.12.003.
Abuzhalihan J, Wang YT, Adi D, et al. Prevalence of dyslipidemia in students from Han, Uygur, and Kazakh ethnic groups in a Medical University in Xinjiang, China. Sci Rep. 2019; 9(1): 19475. doi: 10.1038/s41598-019-55480-5.
Ali N, Kathak RR, Fariha KA, Taher A, Islam F. Prevalence of dyslipidemia and its associated factors among university academic staff and students in Bangladesh. BMC Cardiovasc Disord. 2023; 23(1): 366. doi: 10.1186/s12872-023-03399-1.
Cleeman JI, Grundy SM. National cholesterol Education Program recommendations for cholesterol testing in young adults. A science-based approach. Circulation. 1997; 95: 1646-50.
Washington R.L. Interventions to reduce cardiovascular risk factors in children and adolescents. Am Fam Phys. 1999; 59(8): 2211-8.
World Health Organization Western Pacific Region. The Asia-Pacific perspective: redefining obesity and its treatment. Geneva: World Health Organization; 2000. [cited 2023 Sep 7]. Available from: https://apps.who.int/iris/bitstream/handle/10665/206936/0957708211_eng.pdf.
National cholesterol education program. Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002; 106(25): 3143-421.
Eissa MA, Mihalopoulos NL, Holubkov R, Dai S, Labarthe DR. Changes in fasting lipids during puberty. J Pediatr. 2016; 170: 199-205. doi: 10.1016/j.jpeds.2015.11.018.
Aekplakorn W, Taneepanichskul S, Kessomboon P, et al. Prevalence of dyslipidemia and management in the Thai population, National Health Examination Survey IV, 2009. J Lipids. 2014; 2014: 249584. doi: 10.1155/2014/249584.
Jeenduang N, Whanmasae S, Seepawin P, Kullabootr S. The prevalence of dyslipidemia among a rural Thai population in the Nakhon Si Thammarat province. J Med Assoc Thai. 2013; 96(8): 992-1000.
Theeratrakoolchai O., Chaimanee A. Prevalence of dyslipidemia and associated factors among medical personnel in Nopparat Rajchathani hospital. Thammasat Med J. 2017; 17: 9-17. (in Thai).
Wang L, Wang H, Zhang B, Popkin BM, Du S. Elevated fat intake increases body weight and the risk of overweight and obesity among Chinese adults: 1991-2015 trends. Nutrients. 2020; 12(11): 3272. doi: 10.3390/nu12113272.
Kwon M, Kim J, Cha E. Obesity-status-linked affecting factors of dyslipidemia in Korean youngadult men: based on the Korea national health and nutrition examination survey (2019-2021). Healthcare (Basel). 2023; 11(14): 2015. doi: 10.3390/healthcare11142015.
Klop B, Elte JW, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients. 2013; 5(4): 1218-40. doi: 10.3390/nu5041218.
Wells JC, Fewtrell MS, Williams JE, Haroun D, Lawson MS, Cole TJ. Body composition in normal weight, overweight and obese children: matched casecontrol analyses of total and regional tissue masses, and body composition trends in relation to relative weight. Int J Obes (Lond). 2006; 30(10): 1506-13. doi: 10.1038/sj.ijo.0803402.
Dullaart R, Tol AV. Role of phospholipid transfer protein and prebeta-high density lipoproteins in maintaining cholesterol efflux from Fu5AH cells to plasma from insulin-resistant subjects. Scand J Clin Lab Invest. 2001; 61: 69-74. 10.1080/00365510151068027.
Oda E. LDL cholesterol was more strongly associated with percent body fat than body mass index and waist circumference in a health screening population. Obes Res Clin Pract. 2018; 12(2): 195-203. doi: 10.1016/j.orcp.2017.05.005
Martakis K, Stark C, Rehberg M, Jackels M, Schoenau E, Duran I. Association of muscle mass and fat mass on low-density-lipoprotein cholesterol and triglyceride plasma concentration in children and adolescents. J Pediatr Endocrinol Metab. 2021; 34(10): 1273-82. Published 2021 Jul 19. doi: 10.1515/jpem-2021-0254
Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents, National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 2011; 128(Supl. 5): S213-S256. doi: 10.1542/peds.2009- 2107C.
Klop B., Castro Cabezas M. Chylomicrons: A key biomarker and risk factor for cardiovascular disease and for the understanding of obesity. Curr Cardiovasc Risk Rep. 2012; 6: 27-34. doi: 10.1007/s12170-011-0215-z.
Song P, Zha M, Yang X, et al. Socioeconomic and geographic variations in the prevalence, awareness, treatment and control of dyslipidemia in middle-aged and older Chinese. Atherosclerosis. 2019; 282: 57- 66. doi: 10.1016/j.atherosclerosis.2019.01.005.
Xi Y, Niu L, Cao N, et al. Prevalence of dyslipidemia and associated risk factors among adults aged ≥35 years in northern China: a cross-sectional study. BMC Public Health. 2020; 20(1): 1068. doi: 10.1186/s12889-020-09172-9.
Brinton EA. Effects of ethanol intake on lipoproteins and atherosclerosis. Curr Opin Lipidol. 2010; 21(4): 346-51. doi: 10.1097/MOL.0b013e32833c1f41.