Radiation dose in radiologist from cerebral angiography using optically stimulated luminescence dosimeter
Main Article Content
Abstract
Background: The number of cerebral angiography procedures is increasing, resulting in higher X-ray radiation doses received by radiologists. Consequently, understanding the radiation doses received by radiologists and the accumulation of radiation in control rooms is crucial for guiding prevention strategies against radiation hazards.
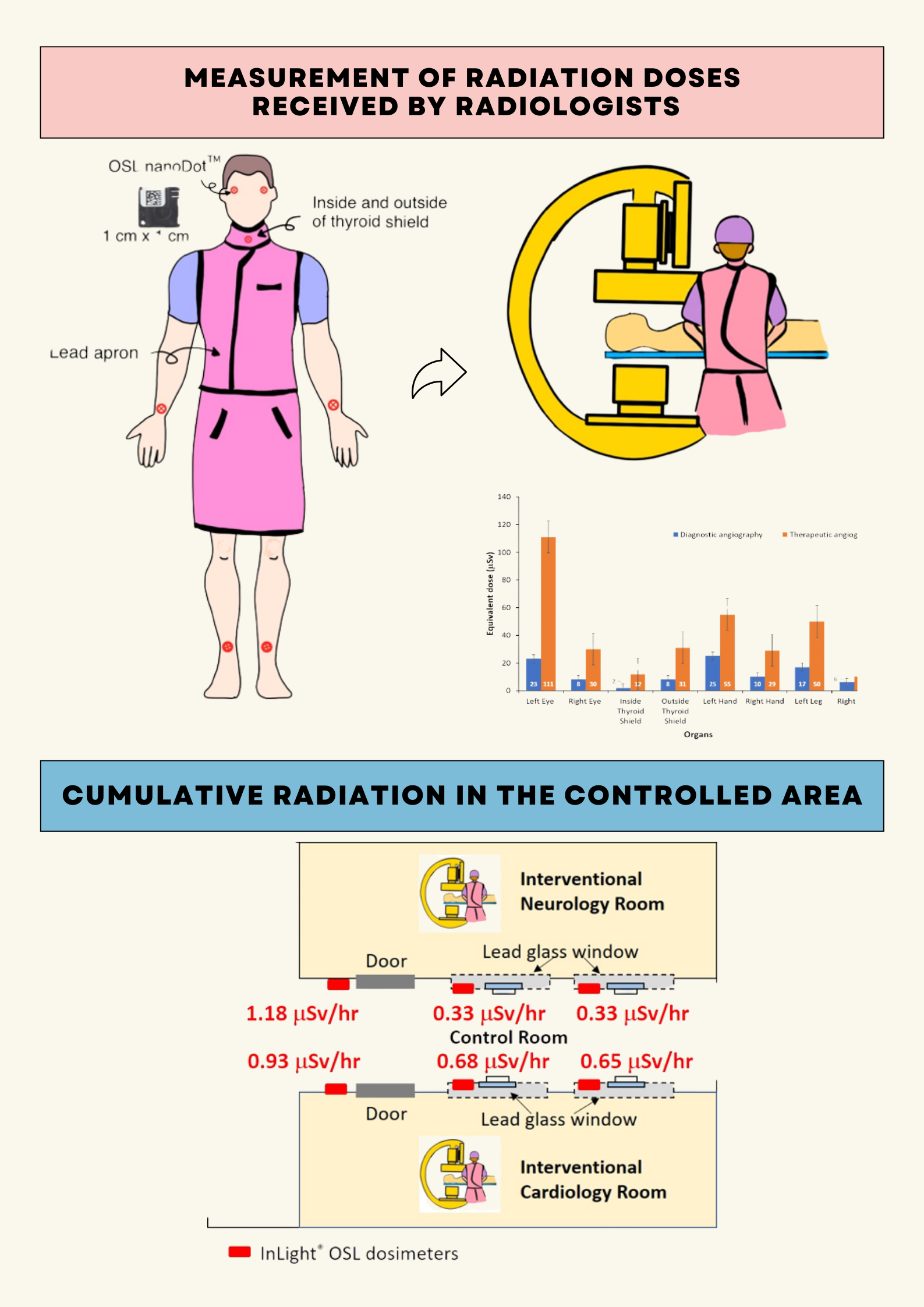
Objectives: This study aimed to measure and evaluate radiation doses to the hands, lenses of the eyes, and thyroids of radiologists performing cerebral angiography procedures, as well as to measure the accumulated radiation dose in the control room.
Materials and methods: OSL dosimeters were placed on the eyeglass frames, thyroids, hands, and legs of radiologists performing 20 cerebral angiography procedures, as well as on the wall and window of the control room.
Results: Radiologists’ average radiation doses were measured at specific body parts as follows: left eye (49 µSv), right eye (15 µSv), left hands (34 µSv), right hands (16 µSv), left legs (27 µSv), right legs (7 µSv), and thyroid glands (14 µSv). Notably, the received doses remained well within the maximum radiation dose limit established by the International Commission on Radiological Protection (ICRP). When calculating the maximum number of procedures that can be performed annually, we based it on the limit of the radiation dose that the eyes’ lenses should not exceed. Our findings revealed that the permissible number of procedures determined by the lens radiation dose limit, should not surpass 405 cases annually (equivalent to 34 cases per month). The radiation dose from therapeutic angiography procedures was discovered to be up to 5 times higher than that from diagnostic angiography procedures. The maximum accumulated radiation dose in the control room was 1.18 µSv/hr, which remained below the limit of the Department of Medical Sciences (< 3 µSv/hr).
Conclusion: Radiologists receive less radiation from cerebral diagnostic angiography than therapeutic angiography. Organs on the left side were exposed to greater radiation levels than those on the right side. Wearing radiation protection devices during each procedure can reduce radiation exposure and mitigate long-term effects on radiologists. It is recommended to monitor and calculate the accumulated radiation dose of workers to ensure their exposure remains within safety limits.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Saposnik G, Galanos LC, Guerrero R, Casagrande F, Adhamidhis E, Gao MMY, et al. The World Stroke Academy: A World Stroke Organization global pathway to improve knowledge in stroke care. Int J Stroke. 2022; 17(8): 829-34. doi: 10.1177/174749 30221085895.
Department of Medical Sciences, Ministry of Public Health. Report on the Situation of NCDs: Diabetes, hypertension and related risk factors in 2019. 1st Ed. Bangkok: Aksorn Graphic and Design Publishing;
(in Thai)
Haussen DC, Nogueira RG. Primer on cerebrovascular diseases: conventional cerebral arteriograph. 2nd Ed. San Diego: Academic Press; 2017: 707-12.
Chida K, Kato M, Kagaya Y, Zuguchi M, Saito H, Ishibashi T, et al. Radiation dose and radiation protection for patients and physicians during interventional procedure. J Radiat Res. 2010; 51(2): 97-105. doi: 10.1269/jrr.09112.
Feygelman VM, Huda W, Peters KR. Effective dose equivalents to patients undergoing cerebral angiography. Am J Neuroradiol. 1992; 13(3): 845-9.
Berthelsen B, Cederblad A. Radiation doses to patients and personnel involved in embolization of intracerebral arteriovenous malformations. Acta Radiol. 1991; 32(6): 492-7. doi: 10.1177/0284185 1910320061.
Lunelli NA, Khoury HJ, Andrade GHV de, Borrás C. Evaluation of occupational and patient dose in cerebral angiography procedures. Radiologia Brasileira. 2013; 46(6): 351–7. doi: 10.1590/S010039842013000600007.
Seals KF, Lee EW, Cagnon CH, Al-Hakim RA, Kee ST. Radiation-induced cataractogenesis: A critical literature review for the interventional radiologist. Cardiovasc Intervent Radiol. 2016; 39(2): 151-60. doi: 10.1007/s00270-015-1207-z.
Authors on behalf of ICRP, Stewart FA, Akleyev AV, Hauer-Jensen M, Hendry JH, Kleiman NJ, et al. ICRP publication 118: ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs--threshold doses for tissue reactions in a radiation protection context. Ann ICRP. 2012; 41(1-2): 1-322. doi:10.1016/j.icrp.2012.02.001.
Gonzales CAB, Morales AA. Assessment of patient and staff doses in interventional cerebral angiography using OSL. Proceedings of World Congress on Medical Physics and Biomedical Engineering; 2015 Jun 7-12; Toronto, Canada, 2015. doi: 10.1007/978-3-319- 19387-8_192.
Moritake T, Matsumaru Y, Takigawa T, Nishizawa K, Matsumura A, Tsuboi K. Dose measurement on both patients and operators during neurointerventional procedures using photoluminescence glass dosimeters. Am J Neuroradiol. 2008; 29(10): 1910-7. doi: 10.3174 /ajnr.A1235.
Castilho AVB, Szjenfeld D, Nalli D, Fornazari V, Moreira AC, Medeiros RB. A study of radiation doses to the patient and medical team at embolization procedures. J Radiat Prot Res. 2019; 44(3): 110-7. doi: 10.14407/jrpr.2019.44.3.110.
Department of Medical Sciences, Ministry of Public Health. Laboratory Radiation Safety Handbook. Bangkok: Beyond Publishing Company Limited; 2020. (in Thai)
Phaorod J, Wongsanon W, Hanpanich P, Dornsrichan P, Awikunprasert P, Sriwicha J, et al. The measurement radiation doses to the lens of eye and thyroid gland from computed tomography brain scans and radiation dose around in CT scan room: phantom study. Srinagarind Med J. 2020; 35(2): 153-60. (in Thai)
Wisetnan C, Molee P, Awikunprasert P, Srichachet K, Pungkun V. A survey of radiation released from patients treated with radioiodine-131 therapy. J Assoc Med Sci. 2021; 54(2): 17-21.doi: 10.14456/ jams.2021.12.
Krisanachinda A, Srimahachota S, Matsubara K. The current status of eye lens dose measurement in interventional cardiology personnel in Thailand. Radiol Phys Technol. 2017; 10(2): 142-7. doi: 10.1007/ s12194-017-0403-8.
Principi S, Delgado Soler C, Ginjaume M, Beltran Vilagrasa M, Rovira Escutia JJ, Duch MA. Eye lens dose in interventional cardiology. Radiat Prot Dosimetry. 2015; 165(1-4): 289-93. doi: 10.1093/ rpd/ncv051.
Palácio EP, Ribeiro AA, Gavassi BM, Di Stasi GG, Galbiatti JA, Junior AD, et al. Exposure of the surgical
team to ionizing radiation during orthopedic surgical procedures. Rev Bras Ortop. 2014; 49(3): 227-32. doi: 10.1016/j.rboe.2014.04.008.
Kaewmarong K, Teebumrung N, Awikunprasert P, Kittichotwarat S, Claimon T, Dachviriyakij T. Measurement of radiation dose by a radiologist from Transarterial Chemoembolization (TACE) intervention with optically stimulated luminescence. J Med Health Sci. 2023; 30(1): 44-52. (in Thai)
Kato M, Chida K, Ishida T, Toyoshima H, Yoshida Y, Yoshioka S, et al. Occupational radiation exposure of the eye in neurovascular interventional physician. Radia Prot Dosim. 2019; 185(2): 151-6. doi: 10.1093/ rpd/ncy285.
Hidajat N, Wust P, Felix R, Schröder RJ. Radiation exposure to patient and staff in hepatic chemoembolization: risk estimation of cancer and deterministic effects. Cardiovasc Intervent Radiol. 2006; 29(5): 791-6. doi: 10.1007/s00270-005-0247-1.