Does mild chronic obstructive pulmonary disease need a standard pulmonary rehabilitation program? A case report
Main Article Content
Abstract
Background: Patients with mild chronic obstructive pulmonary disease (COPD) are usually not recommended for a standard pulmonary rehabilitation (PR)program based on the GOLD guideline in mild COPD GOLD A classification. Especially, the scientific evidence on exercise capacity that can be identified for recruitment in PR programs has been less reported. Thus, a preliminary case study to identify the exercise capacity under cardiopulmonary responses by aerobic exercise testing among patients in mild COPD GOLD A classification was the aim of this study.
Objective: To evaluate the cardiopulmonary responses from exercise capacity testing in individual COPD patients with mild COPD GOLD A Classification.
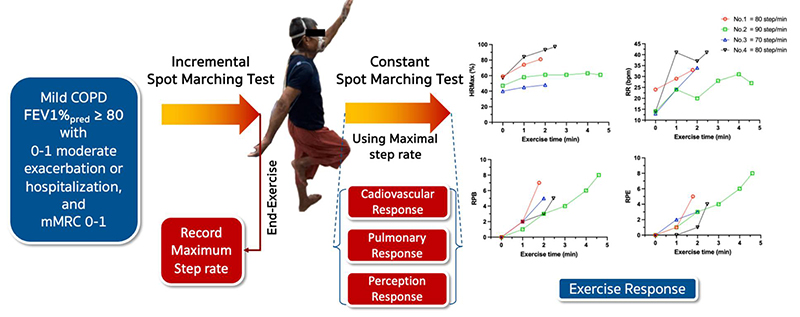
Materials and methods: Four participants with mild COPD GOLD A performed an exercise endurance capacity test at home using Spot Marching Exercise Test (SMT), marching on the spot with high hip and arm raising. The load of SMT was indicated by a controlled stepping rate at 70, 80, 90, 100, and 110 steps/min. Every participant performed Incremental SMT (ISMT) with every 3 min incremental load, and the Constant SMT (CSMT) at the peak load. Both exercise tests were terminated at symptom limit. Resting time between ISMT and CSMT was at least 30 minutes. Cardiopulmonary exercise responses, Borg perceived breathlessness (RPB) and exertion (RPE) were monitored every minute during the exercise test. The duration of exercises was recorded.
Results: Peak exercise capacity using ISMT was low with the end exercise load at 70, 80, 80, and 90 steps/min which is equivalent to moderate to high intensity at 81%, 62%, 65% and 93% of age-predicted maximum heart rate (HRmax). The exercise test was stopped by breathlessness at RPB 7, 8, 6, and 5. Respiratory rates (RR) were 36, 26, 38, and 38 breaths/min. With CSMT, the results showed very short exercise duration 1.78, 4.60, 2.15, and 2.47 mins with RPB 7, 8, 5, and 5 and RR of 33, 27, 34, and 41 breaths/min respectively.
Conclusion: This preliminary report reveals that all four mild COPD GOLD A show low exercise capacity and very poor exercise endurance that should identify the appropriated standard PR program in the future.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Agustí A, Celli BR, Criner GJ, Halpin D, Anzueto A, Barnes P, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am J Respir Crit. 2023; 207(7): 819-37. doi: 10.1183/13993003.00239-2023.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS medicine. 2006; 3(11): e442. doi: 10.1371/journal.pmed.0030442.
Calverley P, Koulouris N. Flow limitation and dynamic hyperinflation: key concepts in modern respiratory physiology. Eur Respir J. 2005; 25(1):186-99. doi: 10.1183/09031936.04.00113204.
Ofir D, Laveneziana P, Webb KA, Lam Y-M, O’Donnell DE. Mechanisms of dyspnea during cycle exercise in symptomatic patients with GOLD stage I chronic obstructive pulmonary disease. Am J Respir Crit. 2008; 177(6):622-9. doi: 10.1164/rccm.200707-1064OC.
O’donnell DE, Laveneziana P, Ora J, Webb KA, Lam YM, Ofir D. Evaluation of acute bronchodilator reversibility in patients with symptoms of GOLD stage I COPD. Thorax. 2009; 64(3):216-23. doi: 10.1136/thx.2008.103598.
Franssen FME, Rochester CL. Comorbidities in patients with COPD and pulmonary rehabilitation: do they matter? Eur Respir Rev. 2014; 23(131):131-41. doi: 10.1183/09059180.00007613.
Rochester CL, Alison JA, Carlin B, Jenkins AR, Cox NS, Bauldoff G, et al. Pulmonary rehabilitation for adults with chronic respiratory disease: an official American thoracic society clinical practice guideline. Am J Respir Crit. 2023; 208(4): e7-e26. doi: 10.1164/rccm.202306-1066ST.
American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) Guidelines for pulmonary rehabilitation programs: Human Kinetics; 2011.
Bolton CE, Bevan-Smith EF, Blakey JD, Crowe P, Elkin SL, Garrod R, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults: accredited by NICE. Thorax. 2013; 68(Suppl 2): ii1-ii30. doi: 10.1136/thoraxjnl2013-203808.
Man W, Chaplin E, Daynes E, Drummond A, Evans RA, Greening NJ, et al. British Thoracic Society Clinical Statement on pulmonary rehabilitation. Thorax. 2023; 78(Suppl 4): s2-s15. doi: 0.1136/thorax-2023-220439.
Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit. 2013; 188(8): e13-64. doi: 10.1164/rccm.201309-1634ST.
McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015; 2015(2): CD003793. doi: 10.1002/14651858.CD003793.pub3.
Hanania NA, O’Donnell DE. Activity-related dyspnea in chronic obstructive pulmonary disease: physical and psychological consequences, unmet needs, and future directions. Int J Chron Obstruct Pulmon Dis. 2019; 14: 1127. doi: 10.2147/COPD.S188141.
Jácome C, Marques A. Pulmonary rehabilitation for mild COPD: a systematic review. Respir Care. 2014; 59(4): 588-94. doi: 10.4187/respcare.02742.
Dejsomritrutai W, Nana A, Maranetra KN, Chuaychoo B, Maneechotesuwan K, Wongsurakiat P, et al. Reference spirometric values for healthy lifetime nonsmokers in Thailand. J Med Assoc Thai. 2000; 83(5): 457-66.
Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am J Respir Crit. 2019; 200(8): e70-e88. doi: 10.1164/rccm.201908-1590ST.
Radtke T, Crook S, Kaltsakas G, Louvaris Z, Berton D, Urquhart DS, et al. ERS statement on standardisation of cardiopulmonary exercise testing in chronic lung diseases. Eur Respir Rev. 2019; 28(154): 180101-25. doi: 10.1183/16000617.0101-2018.
Limphatcharaporn Jirawat, Chidnok Weerapong, Suntrapiwat Kajorn, Jones Chulee. A new cardiopulmonary exercise testing with the Incremental Spot Marching Exercise Test in patients with chronic obstructive pulmonary disease: a pilot study. Thai J Phys Ther. 2020; 42(2): 69-82.
Ubolsakka-Jones C, Jones DA, Pukdeechat M, Boonsawat W, Kritsanapan W, Phimphasak C. Effect of a ConicalPEP Mask on Exercise in Subjects With COPD. Respir Care. 2023; 69(2): 191-201 doi: 10.4187/respcare.11016.
Naosang S, Wannachit N, Jones C. A new endurance exercise test “Spot Brisk Marching”: Lung capacity. Poster session presented at The 8th National Physical Therapy Conferrence. 2016: 20-3.
Gellish RL, Goslin BR, Olson RE, McDonald A, Russi GD, Moudgil VK. Longitudinal modeling of the relationship between age and maximal heart rate. Med Sci Sports Exerc. 2007; 39(5): 822-9. doi: 10.1097/mss.0b013e31803349c6.
Puente-Maestu L, Palange P, Casaburi R, Laveneziana P, Maltais F, Neder JA, et al. Use of exercise testing in the evaluation of interventional efficacy: an official ERS statement. Eur Respir J. 2016; 47(2): 429-60. doi: 10.1183/13993003.00745-2015.
Society AT. ATS statement: guidelines for the sixminute walk test. Am J Respir Crit Care Med. 2002; 166: 111-7. doi: 10.1164/ajrccm.166.1.at1102.
Fotheringham I, Meakin G, Punekar YS, Riley JH, Cockle SM, Singh SJ. Comparison of laboratory-and field-based exercise tests for COPD: a systematic review. Int J Chron Obstruct Pulmon Dis. 2015; 10(1): 625-43. doi: 10.2147/COPD.S70518.
Khaweephab V, Jones C, Phimphasak C, Jones D. Comparison of cardiopulmonary responses between a new spot marching test and six minute walk test in mild to moderate COPD patients. Eur Respiratory Soc; 2016; 48(60): 1592. doi: 10.1183/13993003.congress-2016.PA1592.
Jones C, Phimphasak C, Pukdeechat M, Jones D. Spot Marching Exercise for home-based pulmonary rehabilitation in COPD: physical performance and quality of life. Eur Respiratory Soc; 2018; 52: 3651. doi: 10.1183/13993003.congress-2018.PA3651.
Chidnok W. The suitability of self-paced spot marching exercise as a field endurance test for COPD Chest. 2019; 155(4): 281A. doi.org/10.1016/j.chest.2019.02.271.
Chaw Su Win CJ, Nantinee Nualnim. Cardiopulmonary responses to incremental spot marching exercise test as functional capacity measurement in older adults. International Physical Therapy Research Symposium 2023 (IPTRS 2023); June 8-9, 2023; Khon Kaen University2023. p. 1-11.
O’Donnell DE, Gebke KB. Activity restriction in mild COPD: a challenging clinical problem. Int J Chron Obstruct Pulmon Dis. 2014; 9: 577-88. doi: 10.2147/COPD.S62766.
James MD, Milne KM, Phillips DB, Neder JA, O’Donnell DE. Dyspnea and exercise limitation in mild COPD: the value of CPET. Front Med. 2020; 7: 442. doi: 10.3389/fmed.2020.00442.
Matsuoka S, Washko GR, Dransfield MT, Yamashiro T, Estepar RSJ, Diaz A, et al. Quantitative CT measurement of cross-sectional area of small pulmonary vessel in COPD: correlations with emphysema and airflow limitation. Acad Radiol. 2010; 17(1):93-9. doi: 10.1016/j.acra.2009.07.022.
Rambod M, Porszasz J, Make BJ, Crapo JD, Casaburi R, Investigators COPDGene. Six-minute walk distance predictors, including CT scan measures, in the COPD Gene cohort. Chest. 2012; 141(4): 867-75. doi: 10.1378/chest.11-0870.
O’Donnell DE, Bertley JC, Chau LK, Webb KA. Qualitative aspects of exertional breathlessness in chronic airflow limitation: pathophysiologic mechanisms. Am J Respir Crit. 1997; 155(1): 109-15. doi: 10.1164/ajrccm.155.1.9001298.
O’Donnell DE. Ventilatory limitations in chronic obstructive pulmonary disease. Med Sci Sports Exerc. 2001; 33(7): S647-55. doi: 10.1097/00005768-200107001-00002.
McKeough ZJ, Alison JA, Bye PT. Arm positioning alters lung volumes in subjects with COPD and healthy subjects. Aust J Physiother. 2003; 49(2): 133-7. doi: 10.1016/s0004-9514(14)60129-x.
Laoakka T, Jones C, Khrisanapant W. Inspiratory muscle training increases elevated arm exercise endurance but not 6 minutes walk distance in the elderly. Eur Respir J. 2006; 28(50): 284.