Effect of movement-based priming combined with task specific training on upper limb recovery in patients after stroke
Main Article Content
Abstract
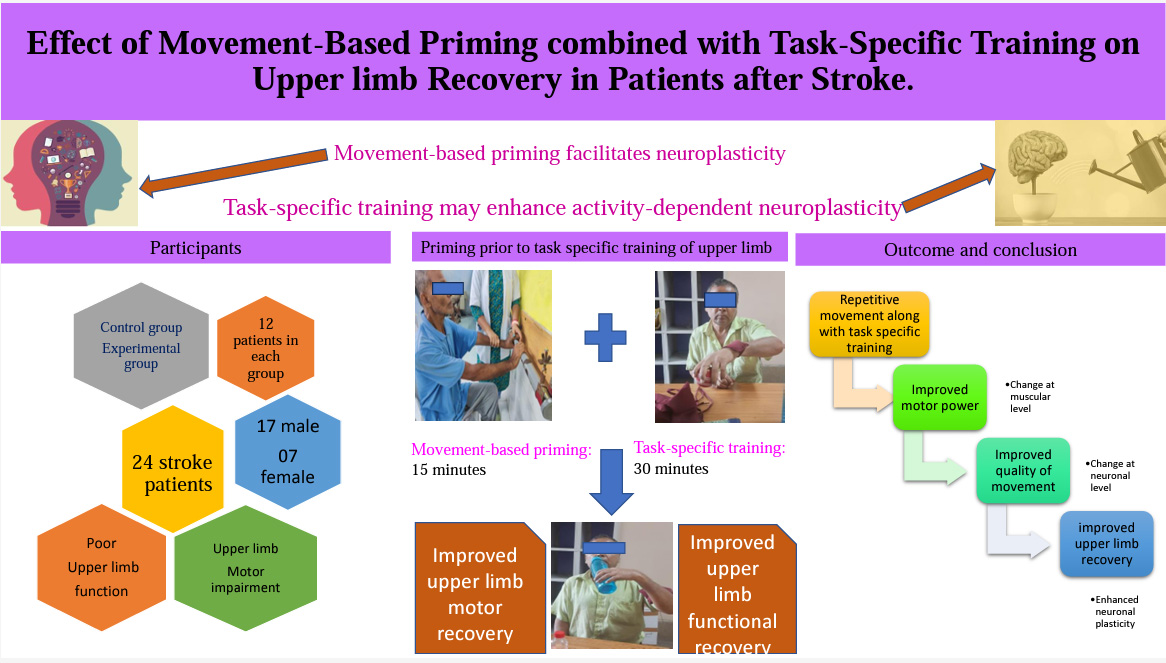
Background: Rehabilitation of upper limb impairments and functional deficits is a top goal in stroke rehabilitation. Alternative therapeutic methods may be developed to facilitate upper limb recovery. Priming prepares the brain for better action. When some therapies accompany Priming, it results in a change in behaviour at the performance level by improving the effect of Neuro-Rehabilitation Therapies and enhancing change in the neural process.
Objectives: To investigate the efficacy of movement-based priming combined with task-specific training on upper limb recovery in patients after stroke.
Materials and methods: Twenty-four subjects in the early phase of stroke, attending the Department of Neurology in a tertiary care hospital of Bhubaneswar, Odisha participated in a single-blind randomized controlled trial. 24 subjects after stroke were recruited to the study and randomly allocated to a control group receiving task-specific training only (TST) and an experimental group receiving Movement-Based Priming with task-specific training (MBP+TST). The control group received only task-specific training for 45 minutes per session three days a week for six weeks, while the experimental group received 15 minutes of priming and 30 minutes of task-specific training. Fugl-Mayer Assessment of upper extremity (FMA-UE)was used to measure upper extremity motor recovery, and the Motor Activity Log (MAL) was used to measure the use of arm and hand during activities of daily living at baseline and after six weeks of therapy.
Results: Both the TST group and the MBP+TST group had significantly improved their capacity to move and use their upper limbs functionally (p<0.001). FMA-UE and MAL scores improved more favorably in the MBP+TST group than in the TST group (p<0.001).
Conclusion: Priming in combination with task-specific training results in better upper limb recovery than task-specific training alone.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Dobkin BH. Rehabilitation after stroke. N Engl J Med. 2005; 352(16): 1677-84.
Horn SD, DeJong G, Smout RJ, Gassaway J, James R, Conroy B. Stroke rehabilitation patients, practice, and outcomes: is earlier and more aggressive therapy better? Arch Phys Med Rehabil. 2005; 86(12): 101- 14. doi: 10.1016/j.apmr.2005.09.016.
Maulden SA, Gassaway J, Horn SD, Smout RJ, DeJong G. Timing of initiation of rehabilitation after stroke. Arch Phys Med Rehabil. 2005; 86(12): 34-40. doi: 10.1016/j.apmr.2005.08.119.
Rodgers H, Mackintosh J, Price C, Wood R, McNamee P, Fearon T, Marritt A, Curless R. Does an early increased-intensity interdisciplinary upper limb therapy programme following acute stroke improve outcome? Clin Rehabil. 2003; 17(6): 579-89. doi: 10.1191/0269 215503cr652oa.
Carey LM, Abbott DF, Egan GF, O’Keefe GJ, Jackson GD, Bernhardt J, Donnan GA. Evolution of brain activation with good and poor motor recovery after stroke. Neurorehabil Neural Repair. 2006; 20(1): 24- 41. doi: 10.1177/1545968305283053.
Stoykov ME, Madhavan S. Motor priming in neurorehabilitation. J Neurol Phys Ther. 2015; 39(1): 33-42. doi: 10.1097/NPT.0000000000000065.
Nowak DA, Grefkes C, Ameli M, Fink GR. Interhemispheric competition after stroke: brain stimulation to enhance recovery of function of the affected hand. Neurorehabil Neural Repair. 2009; 23(7): 641-56. doi: 10.1177/1545968309336661.
Stinear CM, Byblow WD. Modulation of corticospinal excitability and intracortical inhibition during motor imagery is task-dependent. Experimental brain research. Clin Rehabil. 2004; 157: 351-8. doi: 10.1007/s00221-004-1851-z
Ridding MC, McKay DR, Thompson PD, Miles TS. Changes in corticomotor representations induced by prolonged peripheral nerve stimulation in humans. Clin Neuro Physiol. 2001; 112(8): 1461-9.
Conforto, A. B., et al. Effects of somatosensory stimulation on motor function after subacute stroke. Neurorehabili Neural Repair. 2010; 24(3); 263-72. doi: 10.1016/s1388-2457(01)00592-2.
Catani M. A little man of some importance. Brain. 2017; 140(11): 3055-61. doi: 10.1093/brain/awx270.
Stinear CM, Barber PA, Coxon JP, Fleming MK, Byblow WD. Priming the motor system enhances the effects of upper limb therapy in chronic stroke. Brain. 2008; 131(5): 1381-90. doi: 10.1093/brain/awn051.
Stoykov ME, Corcos DM, Madhavan S. Movementbased priming: clinical applications and neural mechanisms. J Mot Behav. 2017; 49(1): 88-97. doi: 10.1080/00222895.2016.1250716
Takebayashi T, Takahashi K, Moriwaki M, Sakamoto T, Domen K. Improvement of upper extremity deficit after constraint-induced movement therapy combined with and without preconditioning stimulation using dual-hemisphere transcranial direct current stimulation and peripheral neuromuscular stimulation in chronic stroke patients: A pilot randomized controlled trial. Front Neurol. 2017; 8: 568. doi: 10.3389/fneur.2017. 00568
Shiner CT, Byblow WD, McNulty PA. Bilateral priming before wii-based movement therapy enhances upper limb rehabilitation and its retention after stroke: a case-controlled study. Neurorehabil Neural Repair. 2014; 28(9): 828-38. doi: 10.1177/1545968314523679.
Stoykov ME, King E, David FJ, Vatinno A, Fogg L, Corcos DM. Bilateral motor priming for post stroke upper extremity hemiparesis: A randomized pilot study. Restor Neurol Neurosci. 2020; 38(1): 11-22. doi: 10.3233/RNN-190943. PMID: 31609714; PMCID: PMC7205167.
Stoykov ME, Biller OM, Wax A, King E, Schauer JM, Fogg LF, Corcos DM. Bilateral upper extremity motor priming (BUMP) plus task-specific training for severe, chronic upper limb hemiparesis: study protocol for a randomized clinical trial. Trials. 2022; 23(1): 1-4.
Hubbard IJ, Vyslysel G, Parsons MW. Interprofessional,
Practice-driven Research: Reflections of One "Community of Inquiry" Based in Acute Stroke. J Allied Health. 2009; 38(2): E69.
Waddell KJ, Birkenmeier RL, Moore JL, Hornby TG, Lang CE. Feasibility of high-repetition, task-specific training for individuals with upper-extremity paresis. The Am J Occup Ther. 2014; 68(4): 444-53. doi: 10.5014/ajot.2014.011619
Birkenmeier RL, Prager EM, Lang CE. Translating animal doses of task-specific training to people with chronic stroke in 1-hour therapy sessions: a proof-ofconcept study. Neuro Rehabil Neural Repair. 2010; 24(7): 620-35. doi: 10.1177/1545968310361957
Stoykov ME, King E, David FJ, Vatinno A, Fogg L, Corcos DM. Bilateral motor priming for post stroke upper extremity hemiparesis: a randomized pilot study. Restor Neurol Neurosci. 2020; 38(1): 11-22. doi: 10.3233/RNN-190943
Carrico C, Chelette KC, Westgate PM, Powell E, Nichols L, Fleischer A, Sawaki L. Nerve stimulation enhances task-oriented training in chronic, severe motor deficit after stroke: a randomized trial. Stroke. 2016; 47(7): 1879-84. doi: 10.1161/STROKEAHA.116.012671.
Patel J, Qiu Q, Yarossi M, Merians A, Massood S, Tunik E, Adamovich S, Fluet G. Exploring the impact of visual and movement based priming on a motor intervention in the acute phase post-stroke in persons with severe hemiparesis of the upper extremity. Disabil Rehabil. 2017; 39(15): 1515-23. doi: 10.1080/09638288.2016.1226419.
Stoykov ME, Stinear JW. Active-passive bilateral therapy as a priming mechanism for individuals in the subacute phase of post-stroke recovery: a feasibility study. Am J Phys Med Rehabil. 2010; 89(11): 873-8. doi: 10.1097/PHM.0b013e3181f1c31c
Stinear CM, Petoe MA, Anwar S, Barber PA, Byblow WD. Bilateral priming accelerates recovery of upper limb function after stroke: a randomized controlled trial. Stroke. 2014; 45(1): 205-10. doi: 10.1161/STROKEAHA.113.003537
Kwakkel G, Kollen BJ, Krebs HI. Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Neurorehabil neural repair. 2008; 22(2): 111-21. doi: 10.1177/1545968307305457.
T.E. Nogles, M.A. Galuska. Middle cerebral artery stroke. StatPearls [Internet]. Treasure Island (FL), StatPearls Publishing (2021). Available from:https://www.ncbi.nlm.nih.gov/books/NBK556132/
Li YC, Lin KC, Chen CL, Yao G, Chang YJ, Lee YY, Liu CT. A Comparative Efficacy Study of Robotic Priming of Bilateral Approach in Stroke Rehabilitation. Front Neurol. 2021; 12: 658567. doi: 10.3389/fneur.2021.658567.
Duncan PW, Propst M, Nelson SG. Reliability of the Fugl-Meyer assessment of sensorimotor recovery following cerebrovascular accident. Phys Ther. 1983; 63(10): 1606-10. doi: 10.1093/ptj/63.10.1606.
Gladstone DJ, Danells CJ, Black SE. The Fugl-Meyer assessment of motor recovery after stroke: A critical review of its measurement properties. Neurorehabil Neural Repair. 2002; 16(3): 232-40. doi: 10.1177/154596802401105171.
Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. A method for evaluation of physical performance. Scand. J Rehabil Med. 1975; 7(1): 13-31.
Taub E, Miller NE, Novack TA, Cook EW, Fleming WC, Nepomuceno CS, Connell JS, Crago JE. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil. 1993; 74(4): 347-54. PMID: 8466415
Stoykov ME, Stinear JW. Active-passive bilateral therapy as a priming mechanism for individuals in the subacute phase of post-stroke recovery: a feasibility study. Am J Phys Med Rehabil. 2010; 89(11): 873. doi: 10.1097/PHM.0b013e3181f1c31c
Hubbard IJ, Parsons MW, Neilson C, Carey LM. Task-specific training: evidence for and translation to clinical practice. OccupTher Int. 2009; 16(3-4): 175- 89. doi: 10.1002/oti.275. PMID: 19504501.
IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.
Yang CL, Lin KC, Chen HC, Wu CY, Chen CL. Pilot comparative study of unilateral and bilateral robotassisted training on upper-extremity performance in patients with stroke. Am J OccupTher. 2012; 66(2): 198-206. doi: 10.5014/ajot.2012.003103.
Hsieh YW, Liing RJ, Lin KC, Wu CY, Liou TH, Lin JC, Hung JW. Sequencing bilateral robot-assisted arm therapy and constraint-induced therapy improves reach to press and trunk kinematics in patients with stroke. J. NeuroEng Rehabil. 2016; 13(1): 1-9. doi: 10.1186/s12984-016-0138-5.
Di Lazzaro V, Profice P, Pilato F, Capone F, Ranieri F, Pasqualetti P, Colosimo C, Pravatà E, Cianfoni A, Dileone M. Motor cortex plasticity predicts recovery in acute stroke. Cereb Cortex. 2010; 20(7): 1523-8. doi: 10.1093/cercor/bhp216
Narayan Arya K, Verma R, Garg RK. Estimating the minimal clinically important difference of an upper extremity recovery measure in subacute stroke patients. Top Stroke Rehabil. 2011; 18(sup1): 599- 610. doi: 10.1310/tsr18s01-599.
da Silva ESM, Ocamoto GN, Santos-Maia GLD, de FátimaCarreira Moreira Padovez R, Trevisan C, de Noronha MA, Pereira ND, Borstad A, Russo TL. The Effect of Priming on Outcomes of Task-Oriented Training for the Upper Extremity in Chronic Stroke: A Systematic Review and Meta-analysis. Neurorehabil Neural Repair. 2020; 34(6): 479-504. doi: 10.1177/1545968320912760.
Uswatte G, Taub E, Morris D, VignoloM, McCulloch K. Reliability and validity of the upper extremity motor activity log-14 for measuring real worldarm use. Stroke. 2005; 36:2493-6. doi: 10.1161/01.STR.0000185928.90848.2e.