Guillain–Barré Syndrome in a patient with systemic lupus erythematosus with underlying pituitary carcinoid: A rare presentation
Main Article Content
Abstract
Background: Guillain-Barré syndrome (GBS) is a rare neuropsychiatric symptom of systemic lupus erythematosus (SLE). GBS in individuals with SLE has distinct features than those without SLE. There is much heterogeneity in the treatment and clinical outcome. Even though GI carcinoids have been related with autoimmune illnesses, extra-gastrointestinal carcinoid coexisting with SLE has been documented only once, and coexistent GBS and SLE with pituitary carcinoid have never been reported previously to the best of our knowledge. Greater knowledge of how inflammation causes cytological alterations that contribute to the formation of a carcinoid might help explore newer pathological mechanisms and therapies.
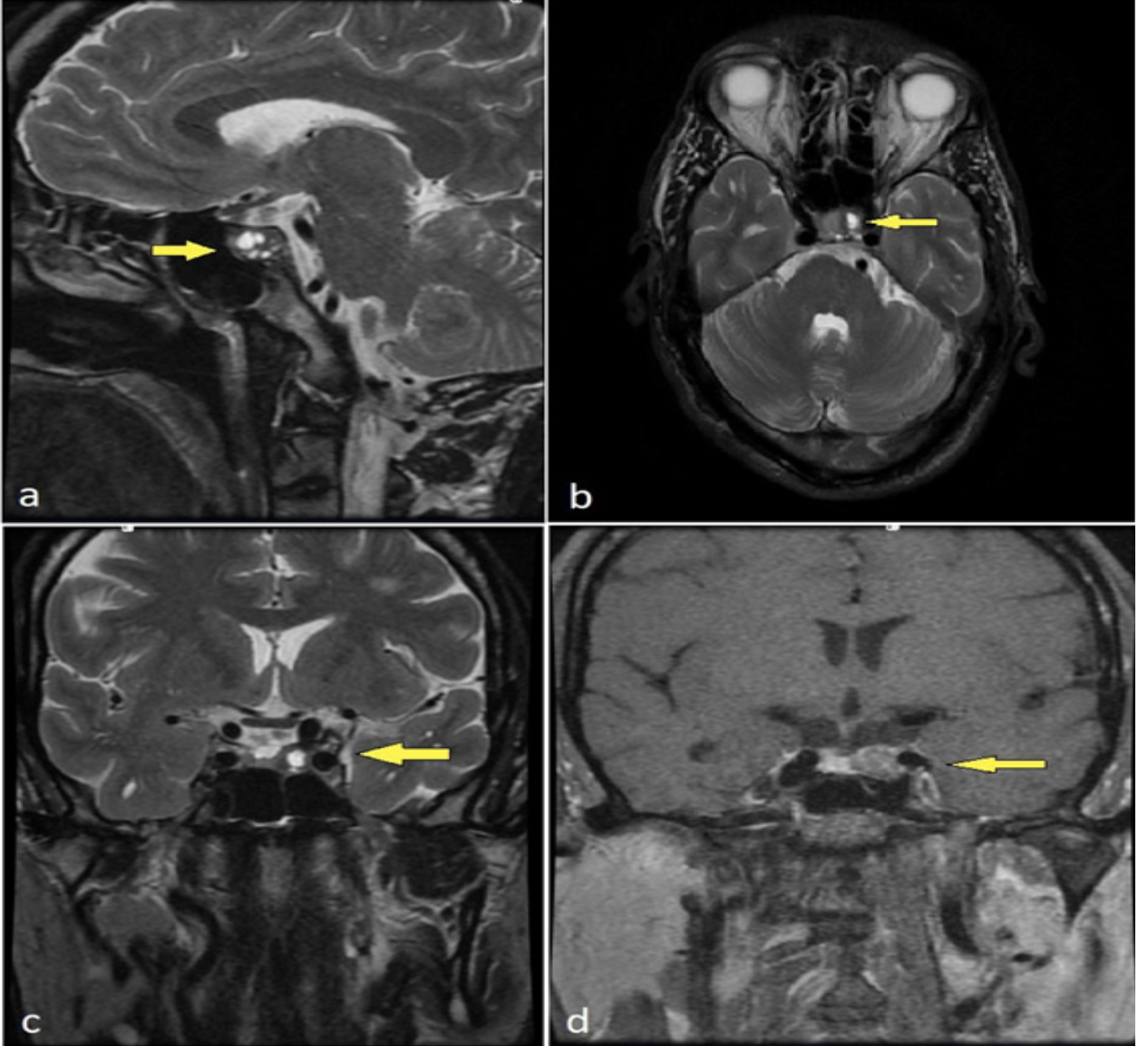
Objectives: We report a middle-aged female who presented with sudden onset of weakness in all four limbs, long-standing history of arthralgia, flushing, dizziness, and a malar rash.
Materials and methods: The initial evaluation led to the diagnosis of GBS and SLE, for which the patient was treated. Further workup of patient revealed the presence of a carcinoid tumor in the pituitary.
Results: Patient was successfully treated with plasmapheresis, steroids, and injection octreotide.
Conclusion: In patients with SLE, neuropsychiatric illness may have a plethora of presentation including GBS. Recognizing such rare presentations and evaluating the possibility of a carcinoid tumor in presence of symptoms like a long-standing history of intermittent palpitation, dizziness, profuse sweating, and flushing, should alert the physician of an underlying carcinoid tumor, which could prove detrimental if left untreated.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Unterman A, Nolte JES, Boaz M, Abady M, Shoenfeld Y, Zandman-Goddard G. Neuropsychiatric syndromes in systemic lupus erythematosus: a meta-analysis. Semin Arthritis Rheum [Internet]. 2011; 41(1): 1-11. https://doi. org/10.1016/j.semarthrit.2010.08.001.
Kakati, S., Barman, B., Ahmed, S. U., & Hussain, M. Neurological manifestations in Systemic Lupus Erythematosus: A single centre study from North East India. J Clin Diagn Res. 2017; 11(1): OC05-OC09. doi:10.7860/JCDR/2017/23773.9280.
Gao, Z., Li, X., Peng, T., Hu, Z., Liu, J., Zhen, J., & Gao, Y. Systemic lupus erythematosus with Guillian-Barre syndrome: A case report and literature review. Medicine. 2018; 97(25): e11160. https://doi.org/10.1097/MD.0000000000011160.
Papadimitraki E, de Bree E, Tzardi M, Skordilis P, Kofteridis D, Tsiftsis DD. Gastriccarcinoid in a young woman with systemic lupus erythemasus and atrophic autoimmune gastritis. Scand J Gastroenterol [Internet]. 2003; 38(5): 477-81. https://doi.org/10.1080/00365520310001734.
Bhambhani, A., Dugar, M., Rao, J., & Prasad, R. Pituitary carcinoid coexisting with systemic lupus erythematosus: A rare combination. The National Medical Journal of India. 2016; 29(4), 209-211.
Santiago-Casas, Y., Peredo, R. A., & Vilá, L. M. Efficacy of low-dose intravenous cyclophosphamide in systemic lupus erythematosus presenting with Guillain-Barré syndrome-like acute axo¬nal neuropathies: report of two cases. Lupus. 2013 : 22(3) : 324-7. https://doi.org/10.1177/ 0961203313476358.
Sarwar, S., Mohamed, A. S., Rogers, S., Sarmast,S. T., Kataria, S., Mohamed, K. H., Singh, R. Neuropsychiatric systemic lupus erythematosus: A 2021 update on diagnosis, management, and current challenges. Cureus. 2021; 13(9): e17969. doi:10.7759/cureus. 17969.
Yuki N, Hartung H-P. Guillain-Barré syndrome. N Engl J Med [Internet]. 2012; 366(24): 2294-304. Available from: http://dx.doi.org/10.1056/NEJMra1114525.
Hanly JG. Neuropsychiatric lupus. Curr Rheumatol Rep [Internet]. 2001; 3(3): 205-12. Available from: http://dx.doi.org/10.1007/s11926-001-0020-7.
Pagnoux, C. Plasma exchange for systemic lupus erythematosus. Transfusion and Apheresis Science: Transfus Apher Sci. 2007; 36(2): 187- 93. doi:10.1016/j.transci.2007.01.004.
Magro-Checa, C., Zirkzee, E. J., Huizinga, T. W., & Steup-Beekman, G. M.Management of neuropsychiatric systemic lupus erythematosus: Current approaches and future perspectives. Drugs. 2016; 76(4): 459-83. doi:10.1007/s40265-015-0534-3.
Neuwelt, C. M. The role of plasmapheresis in the treatment of severe central nervous system neuropsychiatric systemic lupus erythematosus. Therapeutic Apheresis and Dialysis: Ther Apher Dial. 2002; 7(2): 173-82. doi:10.1046/j.1526-0968.2003.00032.x.
Ho, C. M., & Mok, C. C. Therapeutic plasma exchange in patients with systemic lupus erythematosus. J Clin Rheumatol. 2020; 20(02): 65-70. doi:10.1142/s2661341720300062.
Graham, G. W., Unger, B. P., & Coursin, D. B. Perioperative management of selected endocrine disorders. Int Anesthesiol Clin. 2000; 38(4): 31-67. https://doi.org/10.1097/00004311-200010000-00004.
Hemminki, K. &., & Li, X. Incidence trends and risk factors of carcinoid tumours. A national epidemiologic study from Sweden. Cancer. 2001; 92: 2204-10. https://doi. org/10.1002/1097-0142(20011015)92:8<2204::aid-cncr1564>3.0.co;2-r.
Pape, U.-F., Perren, A., Niederle, B., Gross, D., Gress, T., Costa, F., Arnold, R., Denecke, T., Plöckinger, U., Salazar, R., Grossman, A., & Barcelona Consensus Conference participants. ENETS Consensus Guidelines for the management of patients with neuroendocrine neoplasms from the jejuno-ileum and the appendix including goblet cell carcinomas. Neuroendocrinology. 2012; 95(2): 135-56. https:// doi.org/10.1159/000335629.
Nassiri, F., Cusimano, M., Rotondo, F., Horvath, E., & Kovacs, K.Neuroendocrine tumor of unknown origin metastasizing to a growth hormone-secreting pituitary adenoma. World Neurosurgery. 2012; 77(1): 201.e9-201.e12. https://doi. org/10.1016/j.wneu.2011.02.017.
Pinchot, S. N., Holen, K., Sippel, R. S., & Chen, H. Carcinoid tumors. The Oncologist. 2008; 13(12): 1255-69.https://doi.org/10.1634/theoncologist. 2008-0207.
Kwekkeboom, D. J., Krenning, E. P., Lebtahi, R., Komminoth, P., Kos-Kudła, B., de Herder, W. W., Plöckinger, U., Mallorca Consensus Conference participants, & European Neuroendocrine Tumor Society. ENETS Consensus Guidelines for the Standards of Care in NeuroendocrineTumors: peptide receptor radionuclide therapy with radiolabeled somatostatin analogs. Neuroendocrinology. 2009; 90(2): 220-6. https://doi.org/10.1159/000225951.
O’Toole, D., Grossman, A., Gross, D., Delle Fave, G., Barkmanova, J., O’Connor, J., Pape, U.-F., Plöckinger, U., Mallorca Consensus Conference participants, & European Neuroendocrine Tumor Society. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: biochemical markers. Neuroendocrinology. 2009; 90(2): 194-202. https:// doi.org/10.1159/000225948.
Ferolla, P., Faggiano, A., Mansueto, G., Avenia, N., Cantelmi, M. G., Giovenali, P., Del Basso De Caro, M. L., Milone, F., Scarpelli, G., Masone, S., Santeusanio, F., Lombardi, G., Angeletti, G., & Colao, A. The biological characterization of neuroendocrine tumors: the role of neuroendocrine markers. J Endocrinol Invest. 2008; 31(3): 277-86. https:// doi.org/10.1007/BF03345602.
Menda, Y., Ponto, L. L. B., Schultz, M. K., Zamba, G. K. D., Watkins, G. L., Bushnell, D. L., Madsen, M. T., Sunderland, J. J., Graham, M. M., O’Dorisio, T. M., & O’Dorisio, M. S. Repeatabiity of gallium-68 DOTATOC positron emission tomographic imaging in neuroendocrine tumors. Pancreas. 2012; 42(6): 937-43. https://doi.org/10.1097/ MPA.0b013e318287ce21.
Ghevariya, V., Malieckal, A., Ghevariya, N., Mazumder, M., & Anand, S. Carcinoid tumors of the gastrointestinal tract. South Med J. 2009; 102(10):1032-40.https://doi.org/10.1097/ SMJ.0b013e3181b67356.
Modlin, I. M., Oberg, K., Chung, D. C., Jensen, R. T., de Herder, W. W., Thakker, R. V., Caplin, M., Delle Fave, G., Kaltsas, G. A., Krenning, E. P., Moss, S. F., Nilsson, O., Rindi, G., Salazar, R., Ruszniewski, P., & Sundin, A. Gastroenteropancreatic neuroendocrine tumours. The Lancet Oncology. 2008; 9(1): 61-72. https://doi.org/10.1016/S1470-2045(07)70410-2.
Toth-Fejel, S., & Pommier, R. F. (2004). Relationships among delay of diagnosis, extent of disease, and survival in patients with abdominal carcinoid tumors. Am J Surg. 2004; 187(5): 575-9. https:// doi.org/10.1016/j.amjsurg.2004.01.019.