In vitro resistance pattern of Citrobacter infections: A retrospective study
Main Article Content
Abstract
Background: Citrobacter infections are associated with a high mortality rate of about 33-48% if infected patients develop bacteremia. This is partly due to high prevalence of intrinsic resistance, extended spectrum beta lactamases and inducible chromosomal Amp C beta lactamases in Citrobacter spp. thus limiting the therapeutic options. We undertook this study to throw light on the current scenario of infection with this organism.
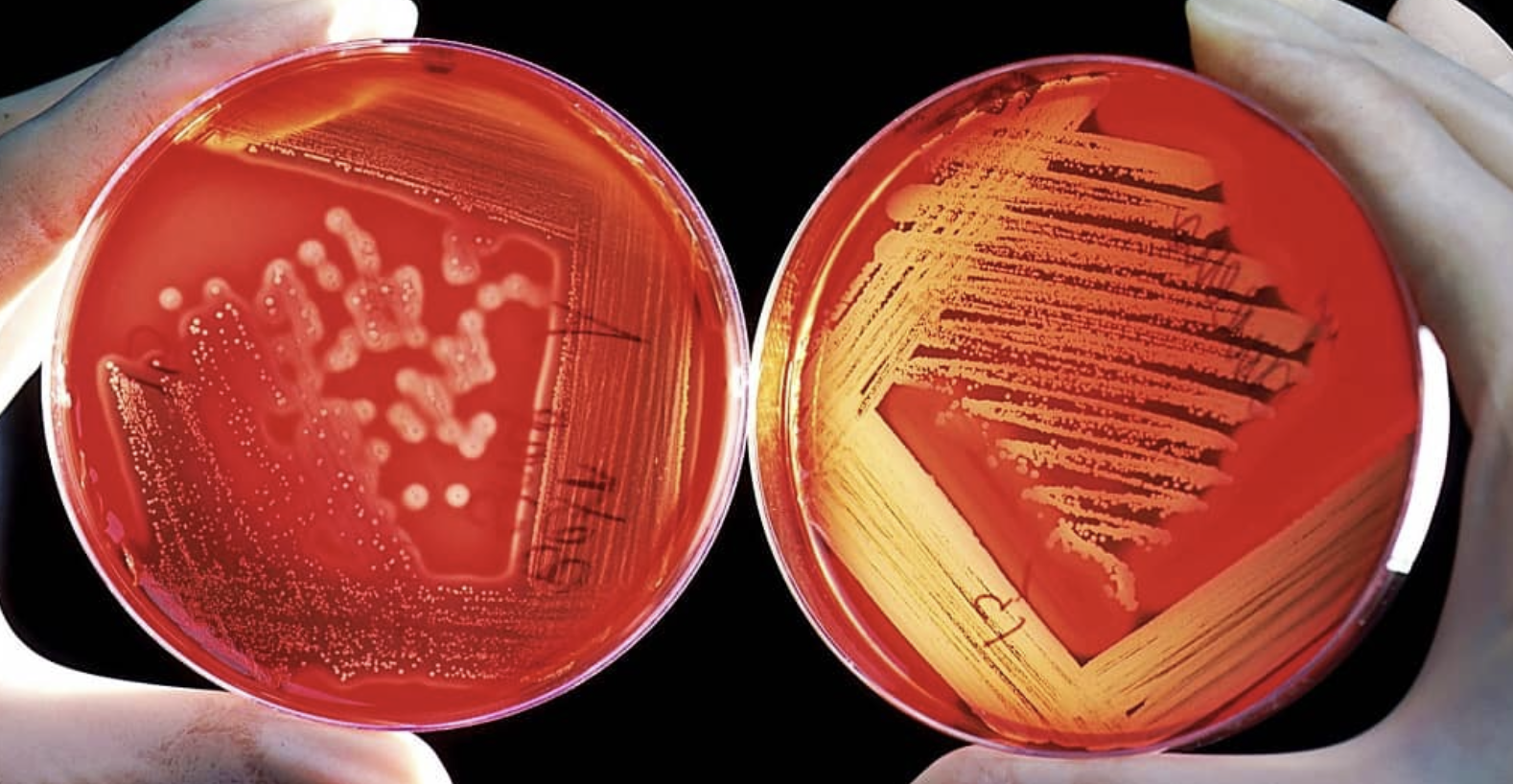
Materials and methods: This retrospective study was conducted over a period of 1 year in Microbiology laboratory of a tertiary care teaching hospital in Eastern part of India. From various samples, 146 clinically significant Citrobacter spp. identified by standard biochemical tests and susceptibility testing performed by Kirby Bauer’s disc diffusion method were included in this study.
Results: Majority of patients age ranged of 41-50 year. The highest number (70/146, 47.9%) of Citrobacter spp. was isolated from pus and wound swabs followed by urine (46/146, 31.5%) and out of these, 51.4% strains were of Citrobacter koseri whereas 48.6% were of Citrobacter fruendii. Of Citrobacter isolates 36.6% were ESBL producers. They showed 54.1%, 37.9%, 47.1%, 39.8% and 58.5% resistance to imipenem, netilmycin, piperacillin tazobactam, minocycline and levofloxacin respectively. We also found 9.6% and 28.4% strains of Citrobacter spp. being resistant to colistin and tigecycline respectively.
Conclusion: Citrobacter spp. showed high degree of resistance to carbapenem and there were colistin resistance strains as well. This study reiterates the emerging resistance in these supposedly low virulence microbes which may pose future challenge in infection control activities.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Nada T, Baba H, Kawamura K, Ohkura T, Torii K, Ohta M. A small outbreak of third generation cephem-resistant Citrobacter freundii infection on a surgical ward. Jpn J Infect Dis. 2004; 57: 181-2.
El Harrif-Heraud Z, Arpin C, Benliman S, Quentin C. Molecular epidemiology of a nosocomial outbreak due to SHV-4- producing strains of Citrobacter diversus. J Clin Microbiol. 1997; 35: 2561-7.
Wang JT, Chang SC, Chen YC and Luh KT. Comparison of antimicrobial susceptibility of Citrobacter freundii isolates in two different time periods. J Microbiol Immunol Infect China. 2000; 33: 258-62.
Gupta N, Yadav A, Choudhury U, Arora DR. Citrobacter bacteremia in a tertiary care hospital. Scan J Infect Dis. 2003; 35(10): 765-8.
Pepperell C, Kus JV, Gardam MA, Humar A and Burrows LL. Low virulence Citrobacter species encode resistance to multiple antimicrobials. Antimicrob Agents Chemother. 2002; 46(11): 3555-60.
Liu L, Wang N , Wu AY, Lin CC ,Lee C M, Liu CP. Citrobacter freundii bacteremia: Risk factors of mortality and prevalence of resistance genes. J Microbiol Immunol Infect. 2018; 51: 565-72.
Collee JG, Miles RS, Wan B. Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and McCartney Practical Medical Microbiology. 14th ed. Edinburgh: Churchill Livingstone; 1996. pp. 131-50.
CLSI. Performance standards for antimicrobial susceptibility testing. 30th edition CLSI Supplement M100. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2020.
Behera B, DasA, Mathur P, KapilA, Gadepalli R, Dhawan B. Tigecycline susceptibility report from an Indian tertiary care hospital. Indian J Med Res. 2009; 129: 446-50.
Lipsky BA, Hook III EW, Smith AA, Plorde JJ. Citrobacter infections in humans: experience at the Seattle Veterans Administration Medical Center and a review of the literature. Rev Infect Dis. 1980; 2: 746-60.
Khanna A, Singh N, Aggarwa AI, Khanna M. The antibiotic resistance pattern in Citrobacter species: An emerging nossocomial pathogen in a tertiary care hospital. J Clin Diagn Res. 2012; 6: 642–4.
Mohanty S, Singhal R, Sood S, Dhawan B, Kapil A, Das BK. Citrobacter infections in a tertiary care hospital in Northern India. J Infect. 2007; 54: 58-64.
Samonis G, Anaissie E, Elting L, Bodey GP. Review of Citrobacter bacteremia in cancer patients over a sixteen-year period. Eur J Clin Microbiol. 1991; 10: 479-85.
Kanamori H, Yano H, Hirakata Y, et al. High prevalence of extended-spectrum ß-lactamases and qnr determinants in Citrobacter species from Japan: Dissemination of CTX-M-2. J Antimicrob Chemother. 2011; 66: 2255-62.
Christo GG, Mathai J, Nalini B, Baliga M, Venkatesh A. Neonatal Citrobacter sepsis: clinical and epidemiological aspects. Indian J Pediatr. 1990; 57: 781-4.
Khadka SB, Thapa B, Mahat K. Nosocomial Citrobacter infection in neonatal intensive care unit in a hospital of Nepal. J Nepal Paediatr Soc. 2010; 31: 105-9.
Metri BC, Jyothi P, Peerapur BV. Anti-microbial resistance profile of Citrobacter species in a tertiary care hospital of Southern India. Indian J Med Sci. 2011; 65: 429-35.
Mohan S, Agarwal J, Srivastava R, Singh M. Observations on Citrobacter species from a tertiary care health center with special reference to multi-drug resistance and presence of CTX-M gene. Indian J Pathol Microbiol. 2014; 5 7: 439-41.
Brenner DJ, Grimont PA, Steigerwalt AG, Fanning GR, Ageron E, Riddle CF. Classification of Citrobacter by DNA hybridization: Designation of Citrobacter farmeri sp. nov. Citrobacter youngae sp. nov. Citrobacter braakii sp. nov. Citrobacter werkmanii sp. nov. Citrobacter sedlakii sp. nov. and three unnamed Citrobacter genomospecies. Int J Syst Bacteriol. 1993; 43: 645-58.
Fernandes R, Amador P, Oliveira C, Prudêncio C. Molecular characterization of ESBL-producing Enterobacteriaceae in northern Portugal. Scientific World Journal. 2014; Article ID782897.
Ali AM, Rafi S, Qureshi AH. Frequency of extended spectrum beta lactamase producing Gram negative bacilli among clinical isolates at clinical laboratories of Army Medical College, Rawalpindi. J Ayub Med Coll Abbottabad. 2004; 16: 35-7.
Praharaj AK, Khajuria A,Kumar M,Grover N. Phenotypic detection and molecular characterization of beta-lactamase genes among Citrobacter species in a tertiary care hospital. Avicenna J Med. 2016; 6(1): 17-27.
Hareendranath G, Dominic R MS, Saralaya V. Clinico-microbiological study of Citrobacter isolates from various clinical specimens and detection of β-lactamase production. Journal of International Medicine and Dentistry. 2015; 2(1): 36-46.
Goossens H, Grabein B. Prevalence and antimicrobial susceptibility data for extended-spectrum beta-lactamase and Amp C- producing Enterobacteriaceae from the MYSTIC Program in Europe and the United States (1997e2004). Diag Microbiol Infect Dis. 2005; 53: 257-64.
Baron EJ, Jones RN. National survey of the in vitro spectrum of piperacillin-tazobactam tested against more than 40,000 aerobic clinical isolates from 236 medical centers. Diag Microbial Infect Dis. 1995; 21:141-51.
Zhang YL, Li JT. The in vitro activity of sulbactam combined with third generation cephalosporin-resistant bacteria. Int J Antimicrob Agents. 2001; 17: 143-6.