The study of bone mass measurement by clavicle radiogrammetry in a comparison to the dual energy x-ray absorptiometry examination
Main Article Content
Abstract
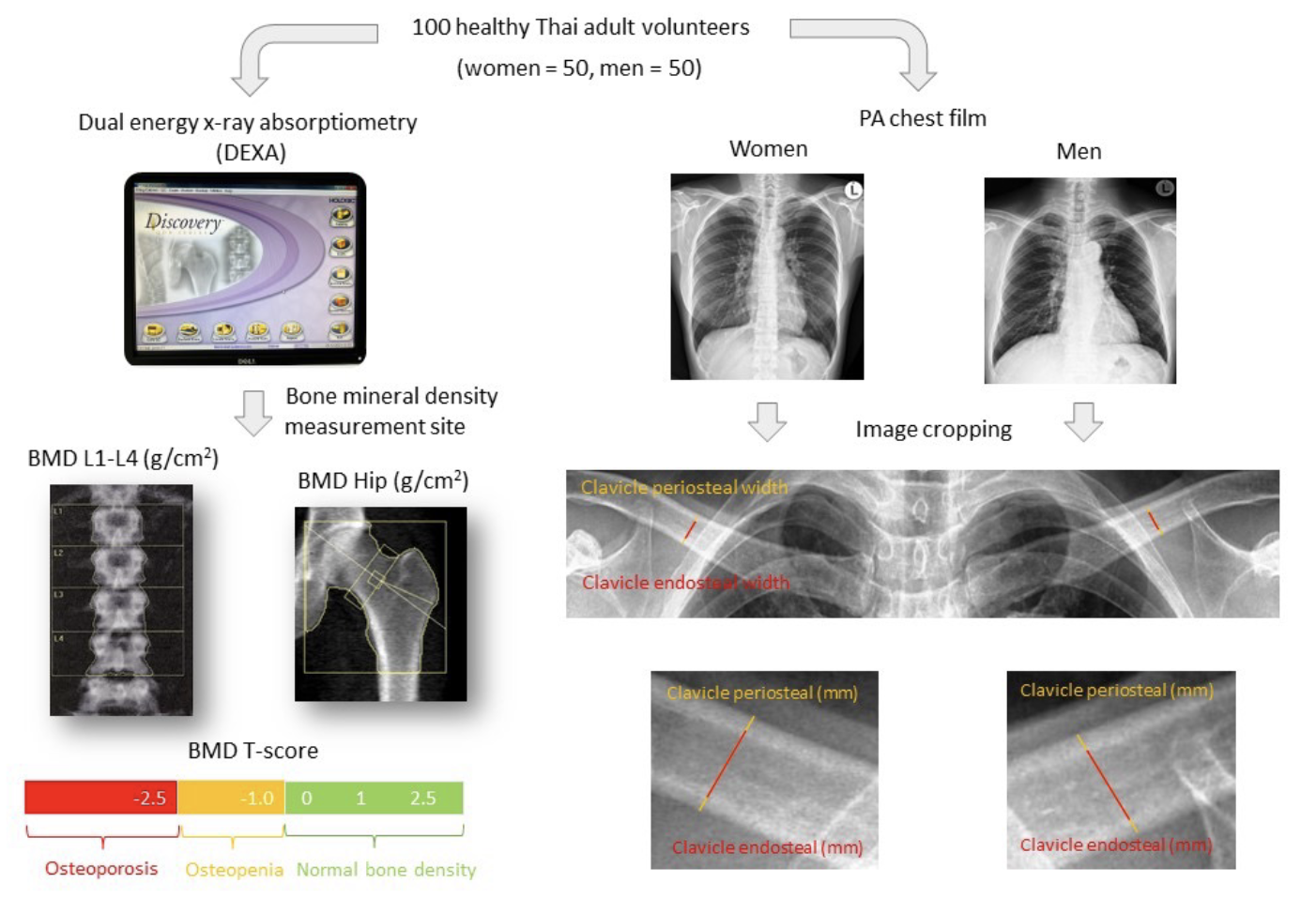
Background: Clavicle radiogrammetry test related to chest radiography has been found to be useful in evaluation of osteoporosis. The diagnosis of osteoporosis was based on the measurement of bone mineral density (BMD) with dual energy x-ray absorptiometry.
Objectives: The aim of this study was to evaluate bone mass measurement using clavicle radiograms to differentiate the goal standards related to the dual energy x-ray absorptiometry methods.
Materials and methods: The population sample consisted of a 100 healthy Thai adult volunteers, (50 women, 50 men) aged from 24 to 76 years. The study subjects were divided as normal bone mass group, T-score ≥ -1.0 and the low bone mass group, T-score ≤ -1.0. Subsequently, posteroanterior (PA) chest radiographs were taken. Measurements of the clavicle radiograms were evaluated, and the images at the midshaft of both clavicles were calculated. An independent t-test was used to examine the differences between the normal and the low bone mass of each gender and two separate BMD sites. The confidence interval was 95% at level of significance 0.05. Pearson’s correlation was used to measure the strength and direction of linear relationship between the bone mass measurement using the dual energy x-ray absorptiometry (DEXA) test and clavicle radiogrammetry test.
Results: The results showed 18 women and 28 men maintained a normal BMD, while 32 women and 22 men had low bone mass density. The average clavicle thickness measurements of the normal bone mass of the women group were lower than the normal bone mass measurements of men. Conversely, the low bone groups of women measurements were higher than low bone mass in the men’s group. A greater diminishing of cortical thickness of clavicle was found in the low bone mass than normal group for both genders. The average cortical thickness of clavicle in the low bone mass of women decreased by 17.8% (5.31 mm/6.46 mm) compared to normal women, while in men, which were fewer, 16.13% (7.07 mm/8.43 mm) between groups, respectively. The average measurements of the clavicle periosteal width and combined cortical thickness of clavicle showed a positive correlation with BMD, whereas, the clavicle endosteal width showed a negative correlation with BMD.
Conclusion: Using the radiogrammetric method to measure the clavicle cortex thickness on the chest x-ray images showed a gradual thinning of the cortex with aging. By comparison, the measurements of clavicle cortex thickness showed a moderate relationship with BMD performed by DEXA in the assessment of osteoporosis.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
Randell A, Sambrook PN, Nguyen TV, Lapsley H, Jones G, Kelly PJ, et al. Direct clinical and welfare costs of osteoporotic fractures in elderly men and women. Osteoporos Int. 1995; 5(6): 427-32. doi: 10.1007/BF01626603.
Pongchaiyakul C, Nguyen ND, Eisman JA, Nguyen TV. Clinical risk indices, prediction of osteoporosis, and prevention of fractures: diagnostic consequences and costs. Osteoporos Int. 2005; 16(11): 1444-50. doi: 10.1007/s00198-005-1996-z.
Heaney RP, Abrams S, Dawson-Hughes B, Looker A, Marcus R, Matkovic V, et al. Peak bone mass. Osteoporos Int. 2000; 11(12): 985-1009. doi: 10.1007/s001980070020.
Osteoporosis prevention, diagnosis, and therapy. NIH consensus statement. 2000; 17(1): 1-45.
Rodin A, Murby B, Smith M, Caleffi M, Fentiman I, Chapman M, et al. Premenopausal bone loss in the lumbar spine and neck of femur: a study of 225 Caucasian women. Bone. 1990; 11(1): 1-5. doi: 10.1016/8756-3282(90)90064-6.
Riggs BL, Melton LJ. Osteoporosis: etiology, diagnosis, and management: Lippincott Williams & Wilkins; 1995.
Doroudinia A, Colletti PM. Bone mineral measurements. Clin Nucl Med. 2015; 40(8): 647-57. doi: 10.1097/RLU.0000000000000860.
Syed Z, Khan A. Bone densitometry: applications and limitations. J Obstet Gynaecol. 2002; 24(6): 476-84. doi: 10.1016/s1701-2163(16)31095-7.
Kumar DA, Anburajan M. The role of hip and chest radiographs in osteoporotic evaluation among south Indian women population: a comparative scenario with DXA. J Endocrinol Invest. 2014; 37(5): 429-40. doi: 10.1007/s40618-014-0074-9.
Delimayanti M. Feature extraction and classification of thorax x-ray image in the assessment of osteoporosis. Proceedings of the 4th International Conference on Electrical, Computer Science and Informatics; 2017; Yogyalarta, Indonesia: IEEE. doi: 10.1109/EECSI.2017.8239102.
Kruger M, Todd J, Schollum L, Kuhn-Sherlock B, McLean D, Wylie K. Bone health comparison in seven Asian countries using calcaneal ultrasound. BMC musculoskeletal disorders. 2013; 14(1): 1-9. doi: 10.1186/1471-2474-14-81.
Ho-Pham LT, T Nguyen UD, Pham HN, Nguyen ND, Nguyen TV. Reference ranges for bone mineral density and prevalence of osteoporosis in Vietnamese men and women. BMC Musculoskelet Disord. 2011; 12(1):1 -7. doi: 10.1186/1471-2474-12-182.
Chen K, Wee S, Pang BWJ, Lau LK, Jabbar KA, Seah WT, et al. Bone Mineral Density Reference Values and Prevalence of Osteoporosis in Singaporean Adults–The Yishun Study. BMC Musculoskelet Disord. 2020;21:633. doi: 10.1186/s12891-020-03646-y.
Chen H, Zhou X, Fujita H, Onozuka M, Kubo K-Y. Age-related changes in trabecular and cortical bone microstructure. Int J Endocrinol. 2013:1687-8337. doi: 10.1155/2013/213234.
Francucci CM, Romagni P, Camilletti A, Fiscaletti P, Amoroso L, Cenci G, et al. Effect of natural early menopause on bone mineral density. Maturitas. 2008; 59(4): 323-8. doi: 10.1016/j.maturitas. 2008.03.008.
Tirosh A, de Souza RJ, Sacks F, Bray GA, Smith SR, LeBoff MS. Sex differences in the effects of weight loss diets on bone mineral density and body composition: POUNDS LOST trial. J Clin Endocrinol Metab. 2015; 100(6): 2463-71. doi: 10.1210/jc.2015-1050.
Wang L, Ran L, Zha X, Zhao K, Yang Y, Shuang Q, et al. Adjustment of DXA BMD measurements for anthropometric factors and its impact on the diagnosis of osteoporosis. Arch Osteoporos. 2020; 15(1): 1-11. doi: 10.1007/s11657-020-00833-1.
Lee J, Lee C, Chung D, Lee H, Park J. Analysis of Age-Based Bone Mineral Density in the Korean Adult Population Using Dual-Energy x-ray Absorptiometry. Applied Sciences. 2020; 10(23): 8469. doi: 10.3390/app10238469.
Saad R, Habli D, El Sabbagh R, Chakhtoura M. Bone health following bariatric surgery: an update. J Clin Densitom. 2020; 23(2): 165-81. doi: 10.1016/j.jocd.2019.08.002.
Maciel J, Araújo I, Trazzi L, Azevedo-Marques P, Salmon C, Paula F, et al. Association of bone mineral density with bone texture attributes extracted using routine magnetic resonance imaging. Clinics. 2020;75:e1766. doi: 10.6061/clinics/2020/e1766.