MRI evaluation of pediatric posterior fossa tumors and its correlation with histopathology: A prospective observational study
Main Article Content
Abstract
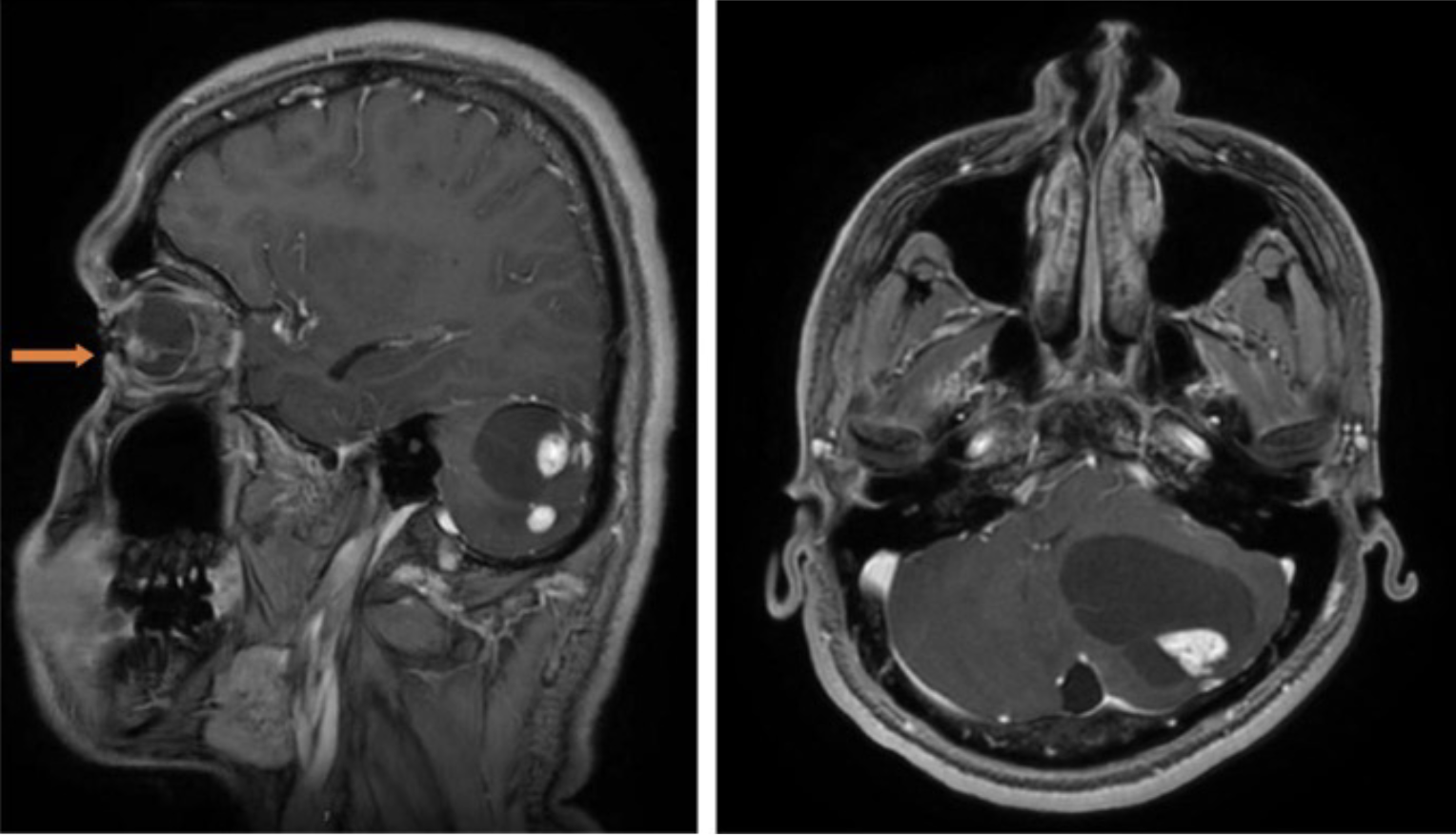
Background: The commonest malignancy in the pediatric age group is leukemia, followed by brain tumors. Pediatric brain tumors are usually seen in children below 10 years. The incidence ranges from 1 to 3 per 100,000 cases. Primary intracranial tumors most commonly occur in the posterior fossa in children while infratentorial tumors are predominant in children over 4 years. Infratentorial tumors are more common overall, accounting for 45-60% of all cases. Physiologic characteristics of the pediatric posterior fossa tumors are well represented in advanced MRI techniques, which results in better pre-operative tumor evaluation, and often better results.
Objectives: Primary intracranial tumors most commonly occur in the posterior fossa in children. Treatment and prognosis rely heavily on correct diagnosis. The most important modality for early diagnosis is MRI of the brain. This study aims to evaluate the role of MRI in pediatric posterior fossa tumors.
Materials and methods: Thirty-three patients in the pediatric age group (<18 years) with a clinical suspicion of posterior fossa tumors, referred to the department of Radiology for undergoing MRI of the brain with contrast were included in the study. These patients underwent surgery followed by histopathological examination (HPE). Five parameters from conventional MRI were chosen and correlated with histopathology (gold standard). Statistical analysis was done subsequently.
Results: Diffusion-weighted imaging (DWI) is the most accurate parameter (94%), followed by T2 weighted imaging (T2WI), gradient, and post-contrast sequence (91% each). Diffusion-weighted imaging and post-contrast sequence had the highest specificity (almost 96%) while DWI and T2WI had the highest sensitivity (90% each). All 5 parameters are useful in 85% of cases. Overall diagnostic accuracy of MRI was almost 94% compared to histopathology.
Conclusion: DWI is the best parameter, followed by T2WI, gradient imaging, and post-contrast sequence. MRI is highly accurate in the evaluation of pediatric posterior fossa tumors. In centers where advanced MRI techniques cannot be performed, some parameters from conventional MRI can be selected that aid in diagnosis. Our study shows that judicious use of 5 parameters can increase sensitivity, specificity, and diagnostic accuracy of MRI for pediatric posterior fossa tumors.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Personal views expressed by the contributors in their articles are not necessarily those of the Journal of Associated Medical Sciences, Faculty of Associated Medical Sciences, Chiang Mai University.
References
O’Brien WT. Imaging of primary posterior fossa brain tumors in children. J Am Osteopath Coll Radiol. 2013; 11; 2(3): 2-12.
Farwell JR, Dohrmann GJ, Flannery JT. Central nervous system tumors in children cns tumors in children. Cancer. 1977; 40(6): 3123-32.
Poretti A, Meoded A, Huisman TA. Neuroimaging of pediatric posterior fossa tumors including review of the literature. J Magn Reson Imaging. 2012; 35(1): 32-47.
Baldwin RT, Preston-Martin S. Epidemiology of brain tumors in childhood—a review. Toxicol appl Pharmacol. 2004; 199(2): 118-31.
Aquilina K. Posterior fossa tumors in children – an overview of diagnosis and management. Adv Clin Neurosci Rehabil. 2013; 13(4): 24-8.
Pollack IF. Brain tumors in children. N Engl J Med. 1994; 331(22): 1500-7.
Plaza MJ, Borja MJ, Altman N, Saigal G. Conventional and advanced MRI features of pediatric intracranial tumors: posterior fossa and suprasellar tumors. Am J Roentgenol. 2013; 200(5): 1115-24.
Ahmad T, Gohar M. MRI evaluation of medulloblastoma with histopahtological correlation. Biomedica. 2014; 30(3) : 1.
Yuh EL, Barkovich AJ, Gupta N. Imaging of ependymomas: MRI and CT. Child's Nerv Syst. 2009; 25(10): 1203-13.
Levy RA, Blaivas M, Muraszko K, Robertson PL. Desmoplastic medulloblastoma: MR findings. Am J Neuroradiol. 1997; 18(7): 1364-6.
Jaremko JL, Jans LB, Coleman LT, Ditchfield MR. Value and limitations of diffusion-weighted imaging in grading and diagnosis of pediatric posterior fossa tumors. Am J Neuroradiology. 2010; 31(9): 1613-6.
Meyers SP, Khademian ZP, Biegel JA, Chuang SH, Korones DN, Zimmerman RA. Primary intracranial atypical teratoid/rhabdoid tumors of infancy and childhood: MRI features and patient outcomes. Am J Neuroradiol. 2006; 27(5): 962-71.
Koeller KK, Rushing EJ. From the archives of the AFIP: medulloblastoma: a comprehensive review with radiologic-pathologic correlation. Radiographics. 2003; 23(6): 1613-37.
Forbes JA, Reig AS, Smith JG, Jermakowicz W, Tomycz L, Shay SD, Sun DA, Wushensky CA, Pearson MM. Findings on preoperative brain MRI predict histopathology in children with cerebellar neoplasms. Pediatr Neurosurg. 2011; 47(1): 51-9.
Camacho AC, Chaljub G, Uribe T, Patterson JT, Swischuk LE. MR Imaging of Pediatric Posterior Fossa Tumors; Contemp Diagn Radiol 2017; 30(14): 1-6.
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P. The 2007 WHO classification of tumors of the central nervous system. Acta Neuropathol. 2007; 114(2): 97-109.
Lee SR, Sanches J, Mark AS, Dillon WP, Norman D, Newton TH. Posterior fossa hemangioblastomas: MR imaging. Radiology. 1989; 171(2): 463-8.