Chinese Herbal Medicine Induced Nephrotoxicity
Main Article Content
Abstract
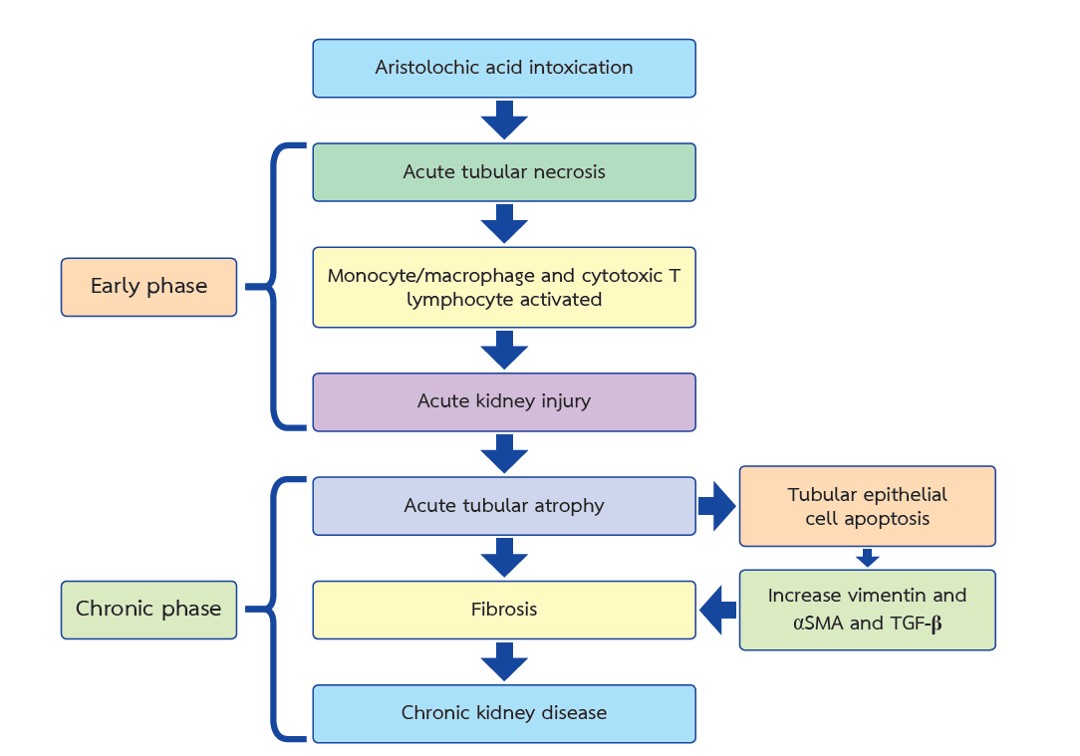
For centuries, Chinese herbal medicine has been used for various purposes, including treating several diseases, aiding in weight reduction, and as food ingredients. The enduring belief is that natural products are safer than modern drugs containing synthetic chemicals. Alternative medicine remains widespread in Thailand today. However, herbs containing compounds like aristolochic acid, other plant alkaloids, and additives from manufacturing processes can cause renal failure. Due to the underreporting of adverse effects, Chinese herbal medicine is often used without caution and with little awareness of potential risks. Renal failure from these herbs can result from mechanisms such as Smad signaling, p53-mediated signaling, and the action of organic anion transporters, leading to apoptosis, fibrosis, and tubular atrophy in the kidneys. Several studies have found that using steroids to treat patients with renal failure caused by Chinese herbal medicines can help slow the progression of kidney failure and reduce the need for renal replacement therapy.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Jadot I, Declèves A-E, Nortier J, Caron N. An Integrated View of Aristolochic Acid Nephropathy: Update of the Literature. Int J Mol Sci. 2017;18(2):297
Debelle FD, Vanherweghem JL, Nortier JL. Aristolochic acid nephropathy: a worldwide problem. Kidney Int. 2008;74(2):158-69.
De Broe ME. Chinese herbs nephropathy and Balkan endemic nephropathy: toward a single entity, aristolochic acid nephropathy. Kidney Int. 2012;81(6):513-5.
Ivić M. Etiology of endemic nephropathy. Lijec Vjesn. 1969;91(12):1273-81.
Luciano RL, Perazella MA. Aristolochic Acid Nephropathy: Epidemiology, Clinical Presentation, and Treatment. Drug Saf. 2015;38(1):55-64.
Chung ACK, Lan HY. Molecular Mechanisms of TGF-β Signaling in Renal Fibrosis. Curr Pathobiol Rep. 2013;1(4):291-9.
Cosyns JP, Jadoul M, Squifflet JP, Wese FX, van Ypersele de Strihou C. Urothelial lesions in Chinese-herb nephropathy. Am J Kidney Dis. 1999;33(6):1011-7.
Ji H, Hu J, Zhang G, Song J, Zhou X, Guo D. Aristolochic acid nephropathy: A scientometric analysis of literature published from 1971 to 2019. Medicine (Baltimore). 2021;100(27):e26510.
Gökmen MR, Cosyns J-P, Arlt VM, Stiborová M, Phillips DH, Schmeiser HH, et al. The Epidemiology, Diagnosis, and Management of Aristolochic Acid Nephropathy. Ann Intern Med. 2013;158(6):469-77.
Nortier JL, Martinez MC, Schmeiser HH, Arlt VM, Bieler CA, Petein M, et al. Urothelial carcinoma associated with the use of a Chinese herb (Aristolochia fangchi). N Engl J Med. 2000;342(23):1686-92.
Baudoux T, Jadot I, Declèves AE, Antoine MH, Colet JM, Botton O, et al. Experimental Aristolochic Acid Nephropathy: A Relevant Model to Study AKI-to-CKD Transition. Front Med (Lausanne). 2022;9:822870.
Vervaet BA, D’Haese PC, Verhulst A. Environmental toxin-induced acute kidney injury. Clin Kidney J. 2017;10(6):747-58.
Vanherweghem JL, Abramowicz D, Tielemans C, Depierreux M. Effects of steroids on the progression of renal failure in chronic interstitial renal fibrosis: a pilot study in Chinese herbs nephropathy. Am J Kidney Dis. 1996;27(2):209-15.
Ma DH, Zheng FL, Su Y, Li MX, Guo MH. Influence and analysis of low-dosage steroid therapy in severe aristolochic acid nephropathy patients. Nephrology (Carlton). 2016;21(10):835-40.
Meyer MM, Chen TP, Bennett WM. Chinese herb nephropathy. Proc (Bayl Univ Med Cent). 2000;13(4):334-7.
Anger EE, Yu F, Li J. Aristolochic Acid-Induced Nephrotoxicity: Molecular Mechanisms and Potential Protective Approaches. Int J Mol Sci. 2020;21(3):1157
Anandagoda N, Lord GM. Preventing aristolochic acid nephropathy. Clin J Am Soc Nephrol. 2015;10(2):167-8.