Effects of Statins Withdrawal on Cardiovascular Events in Chronic Hemodialysis Patients: A Randomized, Triple-blind, Placebo-controlled trial (ESC-HD trial)
Main Article Content
Abstract
Background: The leading cause of death in patients with end stage kidney disease on maintenance hemodialysis (ESKD-D) is a cardiovascular (CV) disease. Efficacy of statins therapy has been proven in non-dialysis patients, but recent guidelines recommend not to initiate statins in ESKD-D patients due to uncertain benefit. However, the clinical outcomes of statins withdrawal in ESKD-D patients previously taken the medications have not been explored.
Method: This is a single-center, prospective, triple-blind, randomized, placebo-controlled trial conducted in ESKD-D patients in Vajira Hospital. The patients were allocated into the statins-withdrawal group, in which the statins were replaced with placebo, and the simvastatin group, in which 20 milligrams per day of simvastatin was prescribed. All participants were followed up for six months with safety interim analysis at 1st and 3rd month. The primary endpoint is the incidence of CV event. The secondary endpoints include serum lipid profile, high-sensitivity C-reactive protein (hs-CRP), high-sensitivity cardiac troponin-T (hs-cTnT), and all-cause mortality.
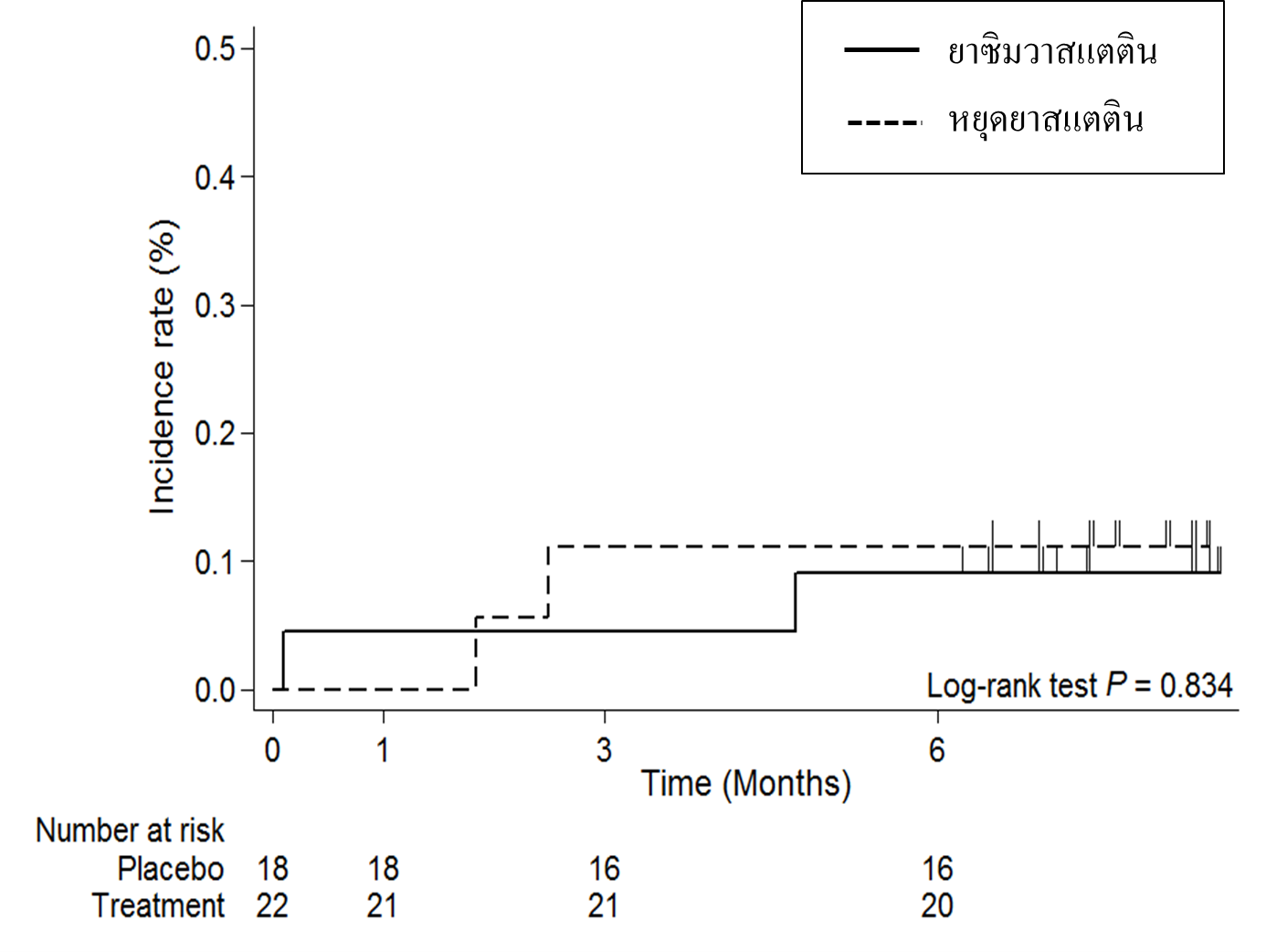
Results: Fortyone participants were included in the study and allocated into the statins-withdrawal group (n = 19) and the simvastatin group (n = 22). One participant was withdrawn from the study. At 6th month, the incidence of CV events was 1.56 and 1.30 per 100 person-months in the statins-withdrawal and the simvastatin group, respectively, which was not statistically different by the Log-rank analysis (p-value=0.834). Total cholesterol and low-density lipoprotein were significantly higher in the statins-withdrawal group at 3rd and 6th months. No difference in hs-CRP and hs-cTnT between groups was detected. No serious adverse events such as hepatitis, rhabdomyolysis, hemorrhagic stroke, or death was reported throughout the study period.
Conclusion: Statins withdrawal in ESKD-D patients significantly increases serum cholesterol level without increasing CV events in the intermediate term. No serious adverse event was reported with simvastatin prescription.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Cozzolino M, Mangano M, Stucchi A, Ciceri P, Conte F, Galassi A. Cardiovascular disease in dialysis patients. Nephrol Dial Transplant. 2018;33:iii28–34.
Herzog CA, Asinger RW, Berger AK, Charytan DM, Díez J, Hart RG, et al. Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2011;80:572–86.
Kilpatrick RD, McAllister CJ, Kovesdy CP, Derose SF, Kopple JD, Kalantar-Zadeh K. Association between Serum Lipids and Survival in Hemodialysis Patients and Impact of Race. J Am Soc Nephrol. 2007;18:293–303.
Liu Y, Coresh J, Eustace JA, Longenecker JC, Jaar B, Fink NE, et al. Association between cholesterol level and mortality in dialysis patients: role of inflammation and malnutrition. JAMA. 2004;291:451–9.
Kidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members. KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 2014;85:1303–9.
Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet. 2011;377:2181–92.
Wanner C, Krane V, März W, Olschewski M, Mann JE, Ruf G, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353:238–48.
Fellström BC, Jardine AG, Schmieder RE, Holdaas H, Bannister K, Beutler J, et al. Rosuvastatin and Cardiovascular Events in Patients Undergoing Hemodialysis. N Engl J Med. 2009;360:1395–407.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Cholesterol Treatment Trialists’ (CTT) Collaboration, Herrington W, Emberson J, Mihaylova B, Blackwell L, Reith C, et al. Impact of renal function on the effects of LDL cholesterol lowering with statin-based regimens: a meta-analysis of individual participant data from 28 randomised trials. Lancet Diabetes Endocrinol. 2016;4:829–39.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73:3168-209.
Golomb BA, Evans MA. Statin adverse effects : a review of the literature and evidence for a mitochondrial mechanism. Am J Cardiovasc Drugs. 2008;8:373–418.
Chow SC, Wang H, Shao J. Sample Size Calculations in Clinical Research. 2nd ed. New York: Chapman and Hall/CRC; 2007.
Chan KE, Thadhani R, Lazarus JM, Hakim RM. Modeling the 4D Study: Statins and Cardiovascular Outcomes in Long-Term Hemodialysis Patients with Diabetes. Clin J Am Soc Nephrol. 2010;5:856–66.
จรณิต แก้วกังวาล, พรรณี ปิติสุทธิธรรม, ชยันต์ พิเชียรสุนทร. ตำราการวิจัยทางคลินิก. กรุงเทพฯ: คณะเวชศาสตร์เขตร้อน มหาวิทยาลัยมหิดล; 2554.
Ridker PM, Danielson E, Fonseca FH, Genest J, Gotto AM, Kastelein JP, et al. Rosuvastatin to Prevent Vascular Events in Men and Women with Elevated C-Reactive Protein. N Engl J Med. 2008;359:2195–207.