Improving Waiting Time in an Oncology Outpatient Clinic at a Tertiary Hospital
Keywords:
Outpatient clinics, Waiting time, oncology, appointments and schedules, Real-world dataAbstract
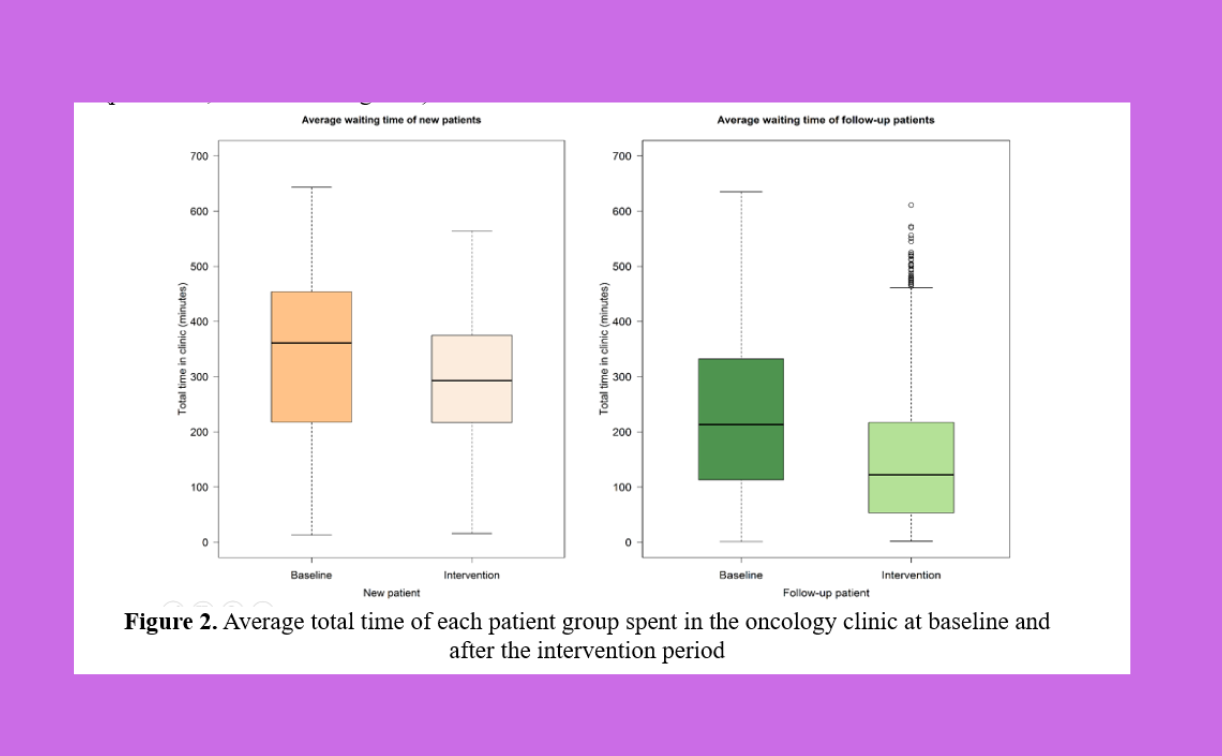
Background: Long waiting times are a common problem in public referral centers. Thus, this study examines the effectiveness of a decision-making scheduling system that was implemented to reduce the waiting time in an oncology outpatient department (OPD) at a tertiary hospital in southern Thailand. Methods: We propose a new scheduling approach based on the Lean management system to reduce OPD waiting time without increasing healthcare resource use. In addition to the scheduled appointment slot, we applied a new scheduling system based on the following three key points: (1) review the necessity of laboratory tests for each patient before the visit date, (2) inform the patient regarding blood draws at arrival and obtain blood results before the doctor’s consultation, and (3) reschedule new patients with their planned treatment start date. Using an in-house electronic hospital information system, we retrospectively reviewed patients who visited oncology OPD between January 2015 and December 2017, then compared the waiting time and number of patient visits before and after implementing the new scheduling system. The waiting time were determined and analyzed by Wilcoxon rank-sum test. Results: The total OPD waiting time of new patients significantly decreased from 361 minutes (interquartile range [IQR] 218.2–454) to 293 minutes (IQR 217–375; p < 0.001). The rate of new patients who received anticancer treatment within two visits was increased from 75.4% to 97% (p < 0.001). Correspondingly, the total OPD waiting time of follow-up patients was also significantly reduced from 213 minutes (IQR 113–332) to 122 minutes (IQR 53–217; p < 0.001). In addition, the new scheduling system reduced the average OPD time by 11.4% (p < 0.001). Conclusion: A decision-making scheduling system based on the use of existing capacity can effectively reduce waiting time in an oncology outpatient clinic.
References
Al-Harajin, R., Al-Subaie, S., & Elzubair, A. (2019). The association between waiting time and
patient satisfaction in outpatient clinics: Findings from a tertiary care hospital in Saudi
Arabia. Journal of Family and Community Medicine, 26(1), 17.
https://doi.org/10.4103/jfcm.JFCM_14_18
Barlow, G. L. (2002). Auditing hospital queuing. Managerial Auditing Journal.
Biya, M., Gezahagn, M., Birhanu, B., Yitbarek, K., Getachew, N., & Beyene, W. (2022). Waiting
time and its associated factors in patients presenting to outpatient departments at Public
Hospitals of Jimma Zone, Southwest Ethiopia. BMC Health Services Research, 22(1),
https://doi.org/10.1186/s12913-022-07502-8
Hamel, L. M., Chapman, R., Eggly, S., Penner, L. A., Tkatch, R., Vichich, J., & Albrecht, T. L.
(2014). Measuring the Use of Examination Room Time in Oncology Clinics: A Novel Approach to Assessing Clinic Efficiency and Patient Flow. Journal of Oncology Practice, 10(6), e385–e389. https://doi.org/10.1200/JOP.2013.001359
Hong, T. S., Shang, P. P., Arumugam, M., & Yusuff, R. M. (2013). Use of simulation to solve
outpatient clinic problems: A review of the literature. South African Journal of Industrial
Engineering, 24(3), 27–42.
International Agency for Research on Cancer. (2021, March). Population Fact Sheet: Thailand.
The Global Cancer Observatory.
Lee, H., Choi, E. K., Min, K. A., Bae, E., Lee, H., & Lee, J. (2022). Physician-Customized
Strategies for Reducing Outpatient Waiting Time in South Korea Using Queueing Theory
and Probabilistic Metamodels. International Journal of Environmental Research and
Public Health, 19(4), 2073. https://doi.org/10.3390/ijerph19042073
Luther, L., Gearhart, T., Fukui, S., Morse, G., Rollins, A. L., & Salyers, M. P. (2017). Working
overtime in community mental health: Associations with clinician burnout and perceived quality of care. Psychiatric Rehabilitation Journal, 40(2), 252–259. https://doi.org/10.1037/prj0000234
Naaz, F., & Mohammed, I. (2019). A time motion study to evaluate the average waiting time in
OPD with reference to patient satisfaction in the setting of state-level AYUSH Hospital
(India). Medical Journal of Islamic World Academy of Sciences, 27(3), 71–76. https://doi.org/10.5505/ias.2019.89410
Oche, M., & Adamu, H. (2013). Determinants of patient waiting time in the general outpatient
department of a tertiary health institution in north Western Nigeria. Annals of Medical
and Health Sciences Research, 3(4), 588–592. https://doi.org/10.4103/2141-9248.122123
R Core Team (2021). (n.d.). R: A language and environment for statistical computing. R
Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
Rosenberg, K., & Mechatie, E. (2018). Overtime Negatively Affects Nurses’ Collaboration with
Coworkers. AJN, American Journal of Nursing, 118(8), 64.
https://doi.org/10.1097/01.NAJ.0000544169.61725.9b
Su, S., & Shih, C.-L. (2003). Managing a mixed-registration-type appointment system in
outpatient clinics. International Journal of Medical Informatics, 70(1), 31–40.
https://doi.org/10.1016/s1386-5056(03)00008-x
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F.
(2021). Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and
Mortality Worldwide for 36 Cancers in 185 Countries. CA: A Cancer Journal for
Clinicians, 71(3), 209–249. https://doi.org/10.3322/caac.21660
Young, T., Brailsford, S., Connell, C., Davies, R., Harper, P., & Klein, J. H. (2004). Using
industrial processes to improve patient care. BMJ (Clinical Research Ed.), 328(7432),
Downloads
Published
Issue
Section
License
Copyright (c) 2024 International Journal of Public Health and Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
If the manuscript is accepted for publication, copyright of the article shall be assigned to the IJPHS. After acceptance of a manuscript, the authors will be requested to complete a copyright transfer agreement form