Calibration of Medical Equipment and Quality Health Care Delivery: A Case of Hospitals in Sunyani Municipality
Keywords:
Calibration Practices , Quality Healthcare, Healthcare System, Confirmatory Factor Analysis, Partial Least SquaresAbstract
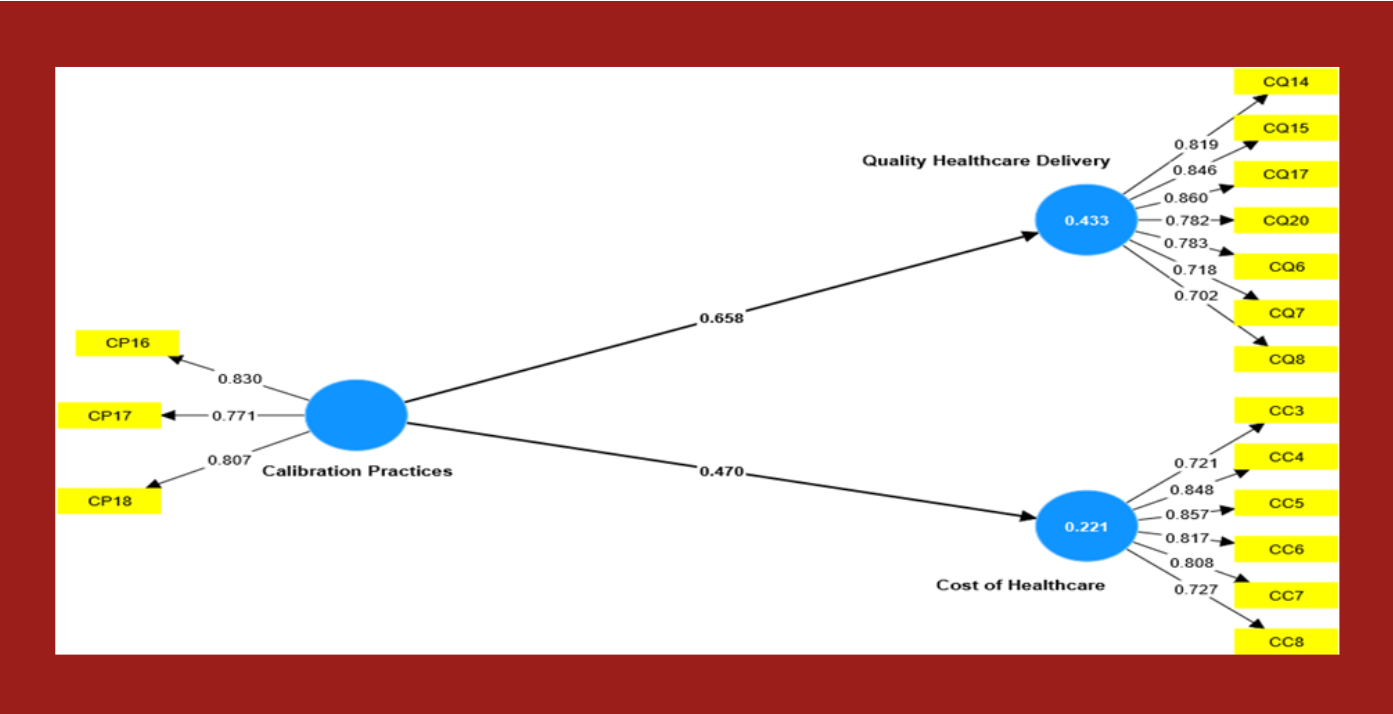
This study examines the impact of medical equipment calibration practices on the delivery of quality healthcare in Sunyani Municipality, encompassing existing procedures, the influence on healthcare quality and costs, and the challenges faced. A quantitative research approach has been utilized for this study. A sample of 394 staff members from the Bono Regional Coordinating Council, Sunyani Municipal Education Directorate, and Sunyani Municipal Assembly was selected using a simple random technique. A structured questionnaire served as the primary data collection instrument. Confirmatory Factor Analysis and Structural Equation Modelling, employing Partial Least Squares methodology, were employed for the data analysis. The findings of this study indicate that rigorous adherence to calibration schedules, coupled with robust quality control measures and ongoing training, is essential for achieving healthcare excellence in municipalities. Furthermore, the study established a significant positive correlation between proper calibration practices and increased healthcare quality, with long-term cost savings being a notable benefit. Despite these positive outcomes, healthcare institutions face challenges such as the lack of standardized protocols and financial constraints, which hinder the effective implementation of these practices. Therefore, this study calls for targeted strategies to enhance awareness and promote technological advancements, paving the way for innovative and quality healthcare in Sunyani Municipality. Future research could delve deeper into these critical aspects, fostering a healthcare system that embodies precision and innovation.
References
Aborujilah, A., Elsebaie, A. E. F. M., & Mokhtar, S. A. (2021). IoT MEMS: IoT-based paradigm for medical equipment management systems of ICUs in light of COVID-19 outbreak. IEEE Access, 9, 131120-131133.
Adam, V. Y., & Nwaogwugwu, J. C. (2020). Availability of personnel, facilities and services in Primary Health Care Centres in a Local Government Area in Benin City, Nigeria. Annals of Clinical and Biomedical Research, 1(1).
Al Awadh, M. (2022). Utilizing Multi-Criteria Decision Making to Evaluate the Quality of Healthcare Services. Sustainability, 14(19), 12745.
Albadr, H. (2019). Designing a decision support system for improving medical devices maintenance in Saudi Arabia (Doctoral dissertation, Brunel University London).
Al-dalahmeh, M., Masa’deh, R., Khalaf, R., & Obeidat, B. (2018). The effect of employee engagement on organizational performance via the mediating role of job satisfaction: the case of it employees in Jordanian banking sector. Modern Applied Science, 12(6), 17. https://doi.org/10.5539/mas.v12n6p17
Asif, M., Jameel, A., Hwang, J., Sahito, N., & Kanwel, S. (2019). Promoting opd patient satisfaction through different healthcare determinants: a study of public sector hospitals. International Journal of Environmental Research and Public Health, 16(19), 3719. https://doi.org/10.3390/ijerph16193719
Aunión-Villa, J., Gómez-Chaparro, M., & García-Sanz-Calcedo, J. (2020). Assessment of the maintenance costs of electro-medical equipment in Spanish hospitals. Expert Review of Medical Devices, 17(8), 855-865. https://doi.org/10.1080/17434440.2020.1796635
Azami, S., Hosseini, S., Alimohammadzadeh, K., Jafari, M., & Bahadori, M. (2021). International sanctions and the procurement of medical equipment in Iran: a qualitative study. Medical Journal of the Islamic Republic of Iran. https://doi.org/10.47176/mjiri.35.180
Bachynsky, N. (2019). Implications for policy: the triple aim, quadruple aim, and interprofessional collaboration. Nursing Forum, 55(1), 54-64. https://doi.org/10.1111/nuf.12382
Bariya, M., Nyein, H. Y. Y., & Javey, A. (2018). Wearable sweat sensors. Nature Electronics, 1(3), 160-171.
Belhouideg, S. (2020). Impact of 3d printed medical equipment on the management of the covid19 pandemic. The International Journal of Health Planning and Management, 35(5), 1014-1022. https://doi.org/10.1002/hpm.3009
Bell, O., Hole, M., Johnson, K., Marcil, L., Solomon, B., & Schickedanz, A. (2020). Medical-financial partnerships: cross-sector collaborations between medical and financial services to improve health. Academic Pediatrics, 20(2), 166-174. https://doi.org/10.1016/j.acap.2019.10.001
Bertoli, P., & Grembi, V. (2017). The political economy of diagnosis-related groups. Social Science & Medicine, 190, 38-47.
Campbell, C. (2004) a Model Clinical Engineering Department Ch. 5 in Clinical Engineering Handbook, Dyro J. Ed. Elsevier Academic Press, Burlington. USA
Cash, R., Rivard, M., Camargo, C., Powell, J., & Panchal, A. (2021). Emergency medical services personnel awareness and training about personal protective equipment during the covid-19 pandemic. Prehospital Emergency Care, 25(6), 777-784. https://doi.org/10.1080/10903127.2020.1853858
Chaudhary, P., & Kaul, P. (2015). Factors affecting utilization of medical diagnostic equipment: A study at a tertiary healthcare setup of Chandigarh. Chrismed: Journal of Health & Research, 2(4).
Chen, C. L., and Yang, T. T., A secure medical data exchange protocol based on cloud environment. J. Med. Syst. 2014. doi: 10.1007/s10916-014-0112-
Cho, H. L. (2019, February). Can Intersectionality Help Lead to More Accurate Diagnosis? The American Journal of Bioethics, 19(2), 37–39. https://doi.org/10.1080/15265161.2018.1557279
Chu, H., Ali, M., & He, Y. (2020). Spatial calibration and pm2.5 mapping of low-cost air quality sensors. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-79064-w
Coon, E., Quinonez, R., Moyer, V., & Schroeder, A. (2014). Overdiagnosis: how our compulsion for diagnosis may be harming children. Pediatrics, 134(5), 1013-1023. https://doi.org/10.1542/peds.2014-1778
Doyle, L., McCabe, C., Keogh, B., Brady, A., & McCann, M. (2019). An overview of the qualitative descriptive design within nursing research. Journal of Research in Nursing, 25(5), 443-455. https://doi.org/10.1177/1744987119880234
Emmanuel, A. and Ibrahim, M. (2022). Efficiency analysis of Syrian refugees’ healthcare services in turkey and other 3rp states. International Journal of Environmental Research and Public Health, 19(22), 14986. https://doi.org/10.3390/ijerph192214986
Faisal, N., Ahmed, R., & Fu, R. (2012). Nano-impact (fatigue) characterization of as-deposited amorphous nitinol thin film. Coatings, 2(3), 195-209. https://doi.org/10.3390/coatings2030195
Gambo, N. and Musonda, I. (2022). Impact of iot towards achieving smart primary healthcare building facilities in Gauteng, south Africa. https://doi.org/10.20944/preprints202207.0228.v1
Ganle, J., Parker, M., Fitzpatrick, R., & Otupiri, E. (2014). A qualitative study of health system barriers to accessibility and utilization of maternal and newborn healthcare services in Ghana after user-fee abolition. BMC Pregnancy and Childbirth, 14(1). https://doi.org/10.1186/s12884-014-0425-8
Garzotto, F., Ceresola, E., Panagiotakopoulou, S., Spina, G., Menotto, F., M, B. & Opocher, G. (2020). Covid-19: ensuring our medical equipment can meet the challenge. Expert Review of Medical Devices, 17(6), 483-489. https://doi.org/10.1080/17434440.2020.1772757
Geta, E., Terefa, D., & Desisa, A. (2023). Efficiency of medical equipment utilization and its associated factors at public referral hospitals in east wollega zone, oromia regional state, ethiopia. Medical Devices Evidence and Research, Volume 16, 37-46. https://doi.org/10.2147/mder.s401041
Ghanouni, A., Meisel, S., Renzi, C., Wardle, J., & Waller, J. (2016). Survey of public definitions of the term ‘overdiagnosis’ in the UK. BMJ Open, 6(4), e010723. https://doi.org/10.1136/bmjopen-2015-010723
Givens, M., Catlin, B., Johnson, S., Pollock, E., Faust, V., Inzeo, P., & Kindig, D. (2020). What do we know about the drivers of health and equity? a narrative review of graphic representations. Health Equity, 4(1), 446-462. https://doi.org/10.1089/heq.2020.0013
Godwin, A. (2023). Supporting healthcare staff after patient safety incidents: An exploration of policy, practice, and terminology: “There’s no point having a rhetoric of concern if nothing will be done” (Doctoral dissertation, Lancaster University).
Gong, G., Chen, Y., Gao, H., Su, D., & Zhang, C. (2019). Has the efficiency of China’s healthcare system improved after healthcare reform? a network data envelopment analysis and tobit regression approach. International Journal of Environmental Research and Public Health, 16(23), 4847. https://doi.org/10.3390/ijerph16234847
Guergov, S. (2022). Investigating e-supply chain issues in internet of medical things (iomt): evidence from the healthcare. International Journal of Computations Information and Manufacturing (Ijcim), 2(2). https://doi.org/10.54489/ijcim.v2i2.110
Gupta, V. and Sarode, S. (2017). Assessment of equipment utilization and maintenance schedule at a dental institution in bengaluru, india. World Journal of Dentistry, 8(2), 104-108. https://doi.org/10.5005/jp-journals-10015-1421
Hinrichs-Krapels, S., Ditewig, B., Boulding, H., Chalkidou, A., Erskine, J., & Shokraneh, F. (2022). Purchasing high-cost medical devices and equipment in hospitals: a systematic review. BMJ Open, 12(9), e057516. https://doi.org/10.1136/bmjopen-2021-057516
Hodgson, T., Magrabi, F., & Coiera, E. (2017). Efficiency and safety of speech recognition for documentation in the electronic health record. Journal of the American Medical Informatics Association, 24(6), 1127-1133. https://doi.org/10.1093/jamia/ocx073
Hollingsworth, A. (2017). Overestimating overdiagnosis in breast cancer screening. Cureus. https://doi.org/10.7759/cureus.966
Hossain, M., Ahmad, M., & Islam, R. (2019). Evaluation of performance outcomes of medical equipment technology management and patient safety: skilled clinical engineer’s approach. Global Clinical Engineering Journal, 1(2), 4-16. https://doi.org/10.31354/globalce.v1i2.46
Humphreys, K., Harris, A., & Weingardt, K. (2008). Subject eligibility criteria can substantially influence the results of alcohol-treatment outcome research. Journal of Studies on Alcohol and Drugs, 69(5), 757-764. https://doi.org/10.15288/jsad.2008.69.757
Hunt, J., Bristowe, K., Chidyamatare, S., & Harding, R. (2017). ‘they will be afraid to touch you’: LGBT people and sex workers' experiences of accessing healthcare in Zimbabwe—an in-depth qualitative study. BMJ Global Health, 2(2), e000168. https://doi.org/10.1136/bmjgh-2016-000168
Ivankova, N. and Wingo, N. (2018). Applying mixed methods in action research: methodological potentials and advantages. American Behavioral Scientist, 62(7), 978-997. https://doi.org/10.1177/0002764218772673
Jansen, L., Schijndel, M., Waarde, J., & Busschbach, J. (2018). Health-economic outcomes in hospital patients with medical-psychiatric comorbidity: a systematic review and meta-analysis. Plos One, 13(3), e0194029. https://doi.org/10.1371/journal.pone.0194029
Kabeta, S., Chala, T., & Tafese, F. (2023). Medical equipment management in general hospitals: experience of Tulu bolo general hospital, south west shoa zone, central Ethiopia. Medical Devices Evidence and Research, Volume 16, 57-70. https://doi.org/10.2147/mder.s398933
Kara, S., Ibrahim, M., & Daneshvar, S. (2021). Dual efficiency and productivity analysis of renewable energy alternatives of OECD countries. Sustainability, 13(13), 7401. https://doi.org/10.3390/su13137401
Karkee, R., Lee, A., & Pokharel, P. (2014). Women’s perception of quality of maternity services: a longitudinal survey in nepal. BMC Pregnancy and Childbirth, 14(1). https://doi.org/10.1186/1471-2393-14-45
Kaur, H., Alam, M., Jameel, R., Mourya, A., & Chang, V. (2018). A proposed solution and future direction for blockchain-based heterogeneous medicare data in cloud environment. Journal of Medical Systems, 42(8). https://doi.org/10.1007/s10916-018-1007-5
Knowles, B. (2016). Emerging trust implications of data-rich systems. IEEE Pervasive Computing, 15(4), 76-84.
Kumar, S., Raut, R., Narwane, V., & Narkhede, B. (2020). Applications of industry 4.0 to overcome the covid-19 operational challenges. Diabetes &Amp; Metabolic Syndrome: Clinical Research &Amp; Reviews, 14(5), 1283-1289. https://doi.org/10.1016/j.dsx.2020.07.010
Li, J., Mao, Y., & Zhang, J. (2023). Construction of medical equipment maintenance network management platform based on big data. Frontiers in Physics, 11. https://doi.org/10.3389/fphy.2023.1105906
Li, R., Asch, S., & Shah, N. (2020). Developing a delivery science for artificial intelligence in healthcare. NPJ Digital Medicine, 3(1). https://doi.org/10.1038/s41746-020-00318-y
Liu, D. and Zhang, F. (2018). Metabolic feedback circuits provide rapid control of metabolite dynamics. Acs Synthetic Biology, 7(2), 347-356. https://doi.org/10.1021/acssynbio.7b00342
Liu, W., Liu, T., Chen, P., Zheng, B., Chien, C., & Tung, T. (2021). Systematic review of the effect of a zero-markup policy for essential drugs on healthcare costs and utilization in china, 2015–2021. Frontiers in Medicine, 8. https://doi.org/10.3389/fmed.2021.618046
Loh, Z., Cheen, M., & Wee, H. (2016). Humanistic and economic outcomes of pharmacist-provided medication review in the community-dwelling elderly: a systematic review and meta-analysis. Journal of Clinical Pharmacy and Therapeutics, 41(6), 621-633. https://doi.org/10.1111/jcpt.12453
Machira, K. and Palamuleni, M. (2018). Women perspectives on quality of maternal health care services in malawi. International Journal of Women S Health, Volume 10, 25-34. https://doi.org/10.2147/ijwh.s144426
Maghzi, P., Mohammadi, M., Pasandide, S., & Naderi, B. (2022). Operating room scheduling optimization based on a fuzzy uncertainty approach and metaheuristic algorithms. International Journal of Engineering, 35(2), 258-275. https://doi.org/10.5829/ije.2022.35.02b.01
Martins, A., Farinha, J., & Cardoso, A. (2020). Calibration and certification of industrial sensors – a global review. Wseas Transactions on Systems and Control, 15, 394-416. https://doi.org/10.37394/23203.2020.15.41
Mason, J. (2018). Surgical intervention and its role in Takayasu arteritis. Best Practice & Research Clinical Rheumatology, 32(1), 112-124. https://doi.org/10.1016/j.berh.2018.07.008
McCauley J. (2004) Maintenance and Repair of Medical Devices Ch.37 in Clinical Engineering Handbook, Dyro J. Ed. Elsevier Academic Press, Burlington. USA, pp 130-132.
McGregor, C., Paton, C., Thomson, C., Chandratilake, M., & Scott, H. (2012). Preparing medical students for clinical decision making: a pilot study exploring how students make decisions and the perceived impact of a clinical decision-making teaching intervention. Medical Teacher, 34(7), e508-e517. https://doi.org/10.3109/0142159x.2012.670323
Menon, R., Wang, A., Chamberlain, K., Harris, L., Li, T., Harris, I., & Adie, S. (2021). Has the reporting of patient‐important outcomes improved in surgical trials? a meta-epidemiological study. Anz Journal of Surgery, 91(10), 2014-2020. https://doi.org/10.1111/ans.16922
Mensah, H. and Oteng-Abayie, E. (2022). Non-probabilistic sampling in quantitative clinical research. International Journal of Applied Research on Public Health Management, 7(1), 1-18. https://doi.org/10.4018/ijarphm.290379
Moyimane, M. and Kekana, M. (2017). Experiences of nurses on the critical shortage of medical equipment at a rural district hospital in south africa: a qualitative study. Pan African Medical Journal, 28. https://doi.org/10.11604/pamj.2017.28.100.11641
Pedersini, F. (2022). Dynamic calibration of triaxial accelerometers with simple setup. Ieee Sensors Journal, 22(10), 9665-9674. https://doi.org/10.1109/jsen.2022.3164362
Phuong, J., Penm, J., Chaar, B., Oldfield, L., & Moles, R. (2019). The impacts of medication shortages on patient outcomes: a scoping review. Plos One, 14(5), e0215837. https://doi.org/10.1371/journal.pone.0215837 pp16-18.
Rahman, N., Ibrahim, A., Hasikin, K., & Razak, N. (2023). Critical device reliability assessment in healthcare services. Journal of Healthcare Engineering, 2023, 1-19. https://doi.org/10.1155/2023/3136511
Rao, S., Xue, H., Teuwen, D., Shi, H., & Yi, H. (2021). Measurements of quality of village-level care and patients’ healthcare-seeking behaviors in rural china. BMC Public Health, 21(1). https://doi.org/10.1186/s12889-021-11946-8
Savitz, L. A. (2016, October). From the Institute for Healthcare Delivery Research. Quality Management in Health Care, 25(4), 248–249. https://doi.org/10.1097/qmh.0000000000000112
Selvaraj, S. (2019). Challenges and opportunities in iot healthcare systems: a systematic review. Sn Applied Sciences, 2(1). https://doi.org/10.1007/s42452-019-1925-y
Sobczak, K. and Leoniuk, K. (2021). Attitudes of medical professionals towards discrimination of patients with obesity. Risk Management and Healthcare Policy, Volume 14, 4169-4175. https://doi.org/10.2147/rmhp.s317808
Sony, M., Antony, J., & McDermott, O. (2022). The impact of medical cyber–physical systems on healthcare service delivery. The TQM Journal, 34(7), 73-93. https://doi.org/10.1108/tqm-01-2022-0005
Steward, K., Kennedy, R., Erus, G., Nasrallah, I., & Wadley, V. (2019). Poor awareness of iadl deficits is associated with reduced regional brain volume in older adults with cognitive impairment. Neuropsychologia, 129, 372-378. https://doi.org/10.1016/j.neuropsychologia.2019.04.023
Storto, C. and Goncharuk, A. (2017). Efficiency vs effectiveness: a benchmarking study on European healthcare systems. Economics & Sociology, 10(3), 102-115. https://doi.org/10.14254/2071-789x.2017/10-3/8
Tang, C. and Abdullah, A. (2016). Can inbound medical tourism boost Malaysia’s economic growth? Tourism and Hospitality Research, 18(4), 505-513. https://doi.org/10.1177/1467358416682069
Vahedi, H., Mirfakhrai, M., Vahidi, E., & Saeedi, M. (2018). Impact of an educational intervention on medical records documentation. World Journal of Emergency Medicine, 9(2), 136. https://doi.org/10.5847/wjem.j.1920-8642.2018.02.009
Velychko, O., Kursin, S., & Gaman, V. (2022). Calibration of high and ultra-high frequency power meters in the range of up to 30 mhz. Measuring Equipment and Metrology, 83(4), 36-42. https://doi.org/10.23939/istcmtm2022.04.036
Walsh, E., Hansen, C., Sahm, L., Kearney, P., Doherty, E., & Bradley, C. (2017). Economic impact of medication error: a systematic review. Pharmacoepidemiology and Drug Safety, 26(5), 481-497. https://doi.org/10.1002/pds.4188
Wang, Y., Perlinger, J., Bartelt-Hunt, S., Kandiah, R., & Ducoste, J. (2018). Another grand challenge: diversity in environmental engineering. Environmental Engineering Science, 35(6), 568-572. https://doi.org/10.1089/ees.2017.0337
Xiaoyi, C., Zhao, Y., Li, Y., Bai, T., Gao, J., & Zhao, C. (2022). Cost-effectiveness of life cycle cost theory-based large medical equipment. Applied Bionics and Biomechanics, 2022, 1-12. https://doi.org/10.1155/2022/8045401
Zamzam, A., Wahab, A., Azizan, M., Satapathy, S., Lai, K., & Hasikin, K. (2021). A systematic review of medical equipment reliability assessment in improving the quality of healthcare services. Frontiers in Public Health, 9. https://doi.org/10.3389/fpubh.2021.753951
Zare, A., Jahangiri, M., Seif, M., Choobineh, A., & Tahernejad, S. (2023). Hand anthropometric survey of iranian healthcare workers. Human Factors and Ergonomics in Manufacturing & Service Industries, 33(4), 338-354. https://doi.org/10.1002/hfm.20994
Zimmermann, N. and Ibaraki, S. (2020). Self-calibration of rotary axis and linear axes error motions by an automated on-machine probing test cycle. The International Journal of Advanced Manufacturing Technology, 107(5-6), 2107-2120. https://doi.org/10.1007/s00170-020-05105-3
Downloads
Published
Issue
Section
License
Copyright (c) 2024 International Journal of Public Health and Health Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
If the manuscript is accepted for publication, copyright of the article shall be assigned to the IJPHS. After acceptance of a manuscript, the authors will be requested to complete a copyright transfer agreement form