Relationship between Duration of Outdoor Activity, Digital Device Usage and Dry Eye in Primary Pterygium
Main Article Content
Abstract
Purpose: This study aimed to evaluate the relationship between time length of outdoor activity, digital devices usage and dry eye conditions in primary pterygium patients.
Setting/Venue: Thammasat University Hospital, Thailand
Method: This study is a population-based, cross-sectional study at Thammasat University Hospital. Demographic characteristics, time spent on outdoor activity, using digital devices and scores for the Ocular Surface Disease Index (OSDI) were collected. The quantitative data was analyzed to determine the mean and relationships by using statistical tools of ANOVA, simple linear regression, and Pearson
correlation.
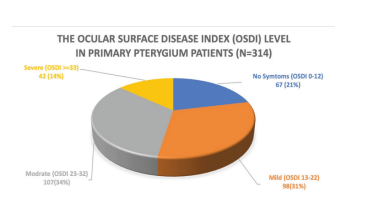
Results: 314 primary pterygium patients were included. An average of 3.46 and 3.64 hours were spent on outdoor activities and digital devices per day respectively. There were 294, 237 and 247 patients (93.63, 75.48, and 78.67 percent) which reported a history of outdoor activity, using digital devices and dry eyes respectively. The study revealed that the time length of outdoor activity had influence on pterygium size, but time of digital devices usage had not. The duration of more than 3 hours of outdoor activity and more than 2 hours of digital devices usage per day were significantly associated with worsening OSDI scores. The relationship between the duration of outdoor activity, digital device usage and the eye pain (R2 = 0.013 and 0.026) and the OSDI scores (R2 = 0.012 and 0.011) were found to be related in the same way.
Conclusion: Primary pterygium patients with a history of outdoor activity and digital devices usage with the duration of more than 3 and 2 hours per day respectively were significantly associated with OSDI scores.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Bradley JC, Yang W, Bradley RH, Reid TW, Schwab IR. The science of pterygia. Br J Ophthalmol 2010;94(7):815-20.
Errais K, Bouden J, Mili-Boussen I, Anane R, Beltaif O, Ouertani AMe. Effect of pterygium surgery on corneal topography. Eur J Ophthalmol 2008;18(2):177-81.
Marmamula S, Khanna RC, Rao GN. Population-Based Assessment of Prevalence and Risk Factors for Pterygium in the South Indian State of Andhra Pradesh: The Andhra Pradesh Eye Disease StudyPterygium in South IndiaAPEDS. Invest Ophthalmol Vis Sci 2013; 54(8):5359-66.
Asokan R, Venkatasubbu RS, Velumuri L, Lingam V, Georgeet R. Prevalence and associated factors for pterygium and pinguecula in a South Indian population. Ophthalmic Physiol Opt 2012;32(1):39-44.
Landers J, Henderson T, Craig J. Prevalence of pterygium in indigenous Australians within central Australia: The Central
Australian Ocular Health Study. Clin Exp Ophthalmol 2011;39(7):604-6.
Pyo EY, Mun GH, Yoon KC. The prevalence and risk factors for pterygium in South Korea: the Korea National Health and Nutrition Examination Survey (KNHANES) 2009-2010. Epidemiol Health 2016;38:2016015.
Sherwin JC, Hewitt AW, Kearns LS, Griffiths LR, Mackey DA, Coroneo MT. The association between pterygium and conjunctival ultraviolet autofluorescence: the Norfolk Island Eye Study. Acta Ophthalmol 2013;91(4):363-70.
Ishioka M, Shimmura S, Yagi Y, Tsubota K. Pterygium and dry eye. Ophthalmologica 2001;215(3):209-11.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf 2017;15(3):276-83.
Schiffman RM, Walt JG, Jacobsen G, Doyle JJ, Lebovics G, Sumneret W, et al.Utility assessment among patients with dry eye disease. Ophthalmology 2003;110(7):1412-9.
Van Tilborg MM, Murphy PJ, Evans KS. Impact of dry eye symptoms and daily activities in a modern office. Optometry
and vision science: official publication of the American Academy of Optometry 2017;94(6):688-93.
Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmology 2018;3(1):000146.
Lekhanont K, Rojanaporn D, Chuck RS, Vongthongsri A. Prevalence of dry eye in Bangkok, Thailand. Cornea 2006;25(10):1162-7.
Phrueksaudomchai P. Vongkittirux S, Kampitak K. Symptoms of ocular surface affecting the daily life in patients with pterygium. Thai J Ophthalmol 2018;70-87.
Kasetsuwan N, Suwan-Apichon O, Lekhanont K, Chuckpaiwong V, Reinprayoon U, Chantra S, et al. Assessing the Risk Factors for Diagnosed Symptomatic Dry Eye Using a Smartphone App: Cross-sectional Study. JMIR mHealth and uHealth 2022;10(6):31011.
Grubbs JR, Tolleson-Rinehart S, Huynh K, Davis RM. A review of quality of life measures in dry eye questionnaires. Cornea
;33(2):215-8.
Phrueksaudomchai P, Tattiyakul W. Prevalence and Associated Factors of Depression in Patients with Pterygium at Thammasat University Hospital. J Med Assoc Thai 2020;103:45.
Phrueksaudomchai P, Tangpakasit W, Kanchanaranya N. Relationship between Time Length of Digital Device Usage and Dry Eye in Pterygium Patients. J Med Assoc Thai 2020;103:27.
Rezvan F, Khabazkhoob M, Hooshmand E, Yekta A, Saatchi M, Hashemi H. Prevalence and risk factors of pterygium: a
systematic review and meta-analysis. Surv Ophthalmol 2018;63(5):719-35.
Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ open ophthalmology 2018;3(1):e000146.