The Comparison of Success Rate in Each Quadrant of Laser Peripheral Iridotomy in Patients with Primary Angle-closure Disease
Main Article Content
Abstract
Background: To find the proper location of LPI based on the success rate in each location regardless of symptoms.
Material and Methods: A retrospective observational study was performed on 57 patients (aged 37-80 years old). All patients were diagnosed with PAC, PACG, or PACS and needed LPI. P values for mean/median data were calculated with the use of the Kruskal Wallis Test, for percentages with the use of Fisher’s exact test.
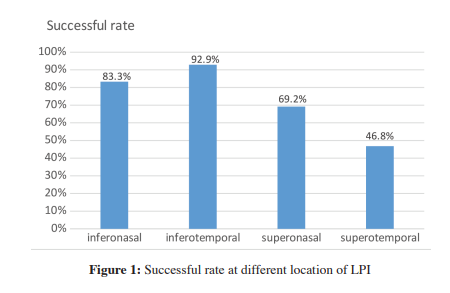
Results: The result shows that the location of PI is statistically related to the success rate (P < .001) with the highest success rate of 92.9% at the inferotemporal area, the inferonasal area with 83.3% successful rate, and the least successful area at the superotemporal part with 46.8%. The laser power and the number of shots used in different locations of PI are not statistically significant.
Conclusions: The success rate of LPI is the highest in the inferotemporal area. There was no clinical difference in dysphotopsia of each quadrant. Therefore, the inferotemporal quadrant could be an alternative in the location of placing laser peripheral iridotomy.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Miki A, Medeiros FA, Weinreb RN, Jain S, He F, Sharpsten L, et al. Rates of retinal nerve fiber layer thinning in glaucoma suspect eyes. Ophthalmology 2014;121(7):1350-8.
Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet 2004;363(9422):1711-20.
Coleman AL, Kodjebacheva G. Risk factors for glaucoma needing more attention. Open Ophthalmol J 2009;3:38-42.
Bourne RR, Sukudom P, Foster PJ, Tantisevi V, Jitapunkul S, Lee PS, et al. Prevalence of glaucoma in Thailand: a population based survey in Rom Klao District, Bangkok. Br J Ophthalmol 2003;87(9):1069-74.
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA 2014:14;311(18):1901-11.
Radhakrishnan S, Chen PP, Junk AK, NouriMahdavi K, Chen TC. Laser Peripheral Iridotomy in Primary Angle Closure:
A Report by the American Academy of Ophthalmology. Ophthalmology 2018;125:1110-20.
Congdon N, Yan X, Friedman DS, Foster PJ, van den Berg TJ, Peng M, et al. Visual symptoms and retinal straylight after laser peripheral iridotomy: the Zhongshan Angle-Closure Prevention Trial. Ophthalmology 2012;119(7):1375-82.
Srinivasan K, Zebardast N, Krishnamurthy P, Abdul Kader M, Raman GV, Rajendrababu S, et al. Comparison of New Visual Disturbances after Superior versus Nasal/Temporal Laser Peripheral Iridotomy: A Prospective Randomized Trial. Ophthalmology 2018;125(3):345-51.
Weintraub J, Berke SJ. Blurring after Iridotomy. Ophthalmology 1992;99(4):479-80.
Vera V, Naqi A, Belovay GW, Varma DK, Ahmed II. Dysphotopsia after temporal versus superior laser peripheral iridotomy: a prospective randomized paired eye trial. Am J Ophthalmol 2014;157(5):929-35.
Congdon N, Yan X, Friedman DS, Foster PJ, Berg TJTP, Peng M, et al. Visual Symptoms and Retinal Straylight after Laser Peripheral Iridotomy. The Zhongshan Angle-Closure Prevention Trial 2012:119(7):1375-82.
Koh V, Keshtkaran MR, Hernstadt D, Aquino MCD, Chew PT, Sng C. Predicting the outcome of laser peripheral iridotomy for primary angle closure suspect eyes using anterior segment optical coherence tomography. Acta Ophthalmol 2019;97(1):57-63.