Immunotactoid glomerulopathy: a case report and literature review
Main Article Content
Abstract
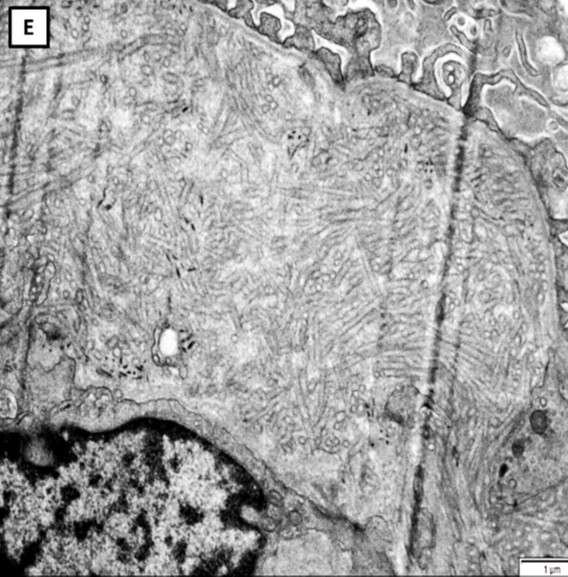
Immunotactoid glomerulopathy (ITG) is a rare glomerular disease, and 90% of patients are Caucasians. The age of patients with ITG ranges from 50 to 70 years, and the certain pathogenesis remains unknown. The ITG is frequently found with lymphoproliferative disorder and monoclonal gammopathy. Patients with ITG usually present edema, proteinuria, microscopic hematuria, hypertension and renal impairment. The overall course typically progresses to end stage renal disease over several years. The renal outcome of ITG depends on hematologic disease treatment. This report describes a 57-year-old Thai man with a history of hypertension and dyslipidemia presenting generalized edema for 6 months. He had proteinuria, microscopic hematuria, poorly controlled blood pressure and renal impairment. Kidney biopsy was performed, and pathologic features were compatible with immunotactoid glomerulopathy. The additional investigations had not detected any hematologic condition. The standard treatment has not been established, so the previously reported treatment was based on the experience of a nephrologist.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
Schwartz MM, Lewis EJ. The Quarterly case: nephrotic syndrome in a middle-aged man. Ultrastruct Pathol. 1980; 1(4):575-82.
Rosenstock JL, Markowitz GS, Valeri AM, Sacchi G, Appel GB, D’Agati VD. Fibrillary and immunotactoid glomerulonephritis: Distinct entities with different clinical and pathologic features. Kidney Int. 2003; 63(4):1450-61.
Bridoux F, Hugue V, Coldefy O, Goujon JM, Bauwens M, Sechet A, et al. Fibrillary glomerulonephritis and immunotactoid (microtubular) glomerulopathy are associated with distinct immunologic features. Kidney Int. 2002; 62(5):1764–75.
Bridoux F, Leung N, Hutchison CA, Touchard G, Sethi S, Fermand JP, et al. Diagnosis of monoclonal gammopathy of renal significance. Kidney Int. 2015; 87(4):698-711.
Alpers CE, Kowalewska J. Fibrillary glomerulonephritis and immunotactoid glomerulopathy. J Am Soc Nephrol. 2008; 19(1):34-7.
Fogo AB, Lusco MA, Najafian B, Alpers CE. AJKD Atlas of renal pathology: Immunotactoid กglomerulopathy. Am J Kidney Dis. 2015; 66(4):e29-30.
Nasr SH, Fidler ME, Cornell LD, Leung N, Cosio FG, Sheikh SS, et al. Immunotactoid glomerulopathy: clinicopathologic and proteomic study. Nephrol Dial Transplant. 2012; 27(11):4137-46.
Jain A, Haynes R, Kothari J, Khera A, Soares M, Ramasamy K. Pathophysiology and management of monoclonal gammopathy of renal significance. Blood Adv. 2019; 3(15):2409–23.
Nasr SH, Kudose SS, Said SM, Santoriello D, Fidler ME, Williamson SR, et al. Immunotactoid glomerulopathy is a rare entity with monoclonal and polyclonal variants. Kidney Int. 2021; 99(2):410-20.
Schwartz MM, Korbet SM, Lewis EJ. Immunotactoid glomerulopathy. J Am Soc Nephrol. 2002; 13(5): 1390-7.
Rosenmann E, Eliakim M. Nephrotic syndrome associated with amyloid-like glomerular deposits. Nephron. 1977;18(5):301-8.
Korbet SM, Schwartz MM. Immunotactoid glomerulopathy. Am J Kidney Dis. 1991; 17(3):247-57.
Jain S, Chhabra D. A case of immunotactoid glomerulopathy with rapid progression to end-stage renal disease. Scientific World Journal. 2009; 9: 1348-54.
Salvadori M, Tsalouchos A. New aspects of fibrillary and immunotactoid glomerulonephritis. EMJ Nephrol. 2019; 7(1):78-84.
Li C, Ruotsalainen V, Tryggvason K, Shaw AS, Miner JH. CD2AP is expressed with nephrin in developing podocytes and is found widely in mature kidney and elsewhere. Am J Physiol Renal Physiol. 2000; 279(4):F785-92.
Alpers CE, Kowalewska J. Fibrillary glomerulonephritis and immunotactoid glomerulopathy. J Am Soc Nephrol. 2008; 19(1):34-7.
Andeen NK, Yang HY, Dai DF, MacCoss MJ, Smith KD. DNAJ homolog subfamily B member 9 is a putative autoantigen in fibrillary GN. J Am Soc Nephrol. 2018; 29(1):231-9.
Ohashi A, Kumagai J, Nagahama K, Fujisawa H. Case of immunotactoid glomerulopathy showing high responsiveness to steroids therapy despite severe pathological features. BMJ Case Rep. 2019; 12(7):e229751.
Javaugue V, Dufour-Nourigat L, Desport E, Sibille A, Moulin B, Bataille P, et al. Results of a nation-wide cohort study suggest favorable long-term outcomes of clone-targeted chemotherapy in immunotactoid glomerulopathy. Kidney Int. 2021; 99(2):421-30.
Alpers CE, Rennke HG, Hopper J, Biava CG. Fibrillary glomerulonephritis: An entity with unusual immunofluorescence features. Kidney Int. 1987; 31(3):781-9.
Korbet S, Rosenberg F, Schwartz MM, Lewis EJ. Course of renal transplantation in immunotactoid glomerulopathy. Am J Med. 1990; 89(1):91-5.
Miki K, Sumida M, Iwadoh K, Honda K, Murakami T, Koyama I, et al. Recurrence of immunotactoid glomerulopathy with monoclonal IgG3к deposits after kidney transplant. Arch Organ Transplant 2017;2(1):015-018.
Carles X, Rostaing L, Modesto A, Orfila C, Cisterne JM, Delisle MB, et al. Successful treatment of recurrence of immunotactoid glomerulopathy in a kidney allograft recipient. Nephrol Dial Transplant. 2000; 15(6):897-900.
Sathyan S, Khan FN, Ranga KV. A Case of recurrent immunotactoid glomerulopathy in an allograft treated with rituximab. Transplant Proc. 2009; 41(9):3953-5.