Catheter-related bloodstream infection
Main Article Content
Abstract
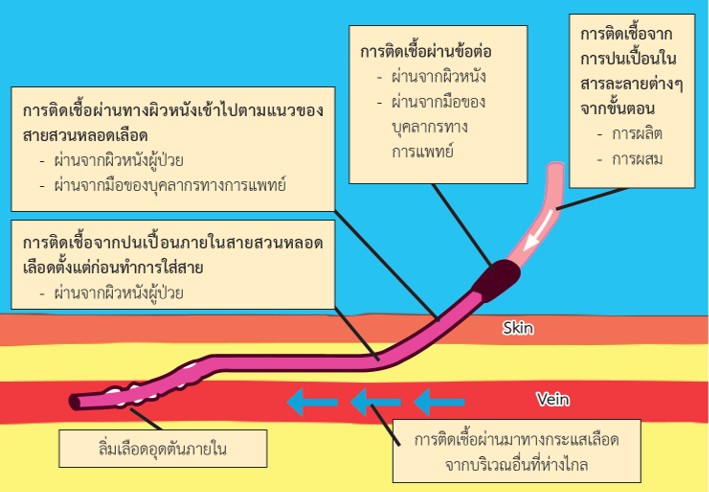
Catheter-related blood stream infections (CRBSI) are among the common complications encountered in patients with end stage renal disease (ESRD) who received hemodialysis with central venous catheters. CRBSI can cause disability, increased morbidity and mortality, longer length of hospital stays as well as increased health care costs in these patients. Here in, we reviewed with regard to definition, the mechanism of infection, the etiology and organisms involved, the types of infections, the treatment of CRBSI, and the preventive measures. As of today, previous studies demonstrate many preventive measures e.g., use of antibiotic locks, shower safety, nares decolonization and using chlorhexidine caps. The aim of all these preventive measures is to decrease the rate of infection with proper efficiency, cost-effectiveness and convenience without increasing in the incidence of antibiotic resistance nor decreasing in duration of use of catheters. All preventive measure should be applied to everyday practice in hemodialysis unit.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This article is published under CC BY-NC-ND 4.0 license, which allows for non-commercial reuse of the published paper as long as the published paper is fully attributed. Anyone can share (copy and redistribute) the material in any medium or format without having to ask permission from the author or the Nephrology Society of Thailand.
References
United States Renal Data System. 2019 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2019.
Nguyen DB, Shugart A, Lines C, Shah AB, Edwards J, Pollock D et al. National healthcare safety network (NHSN) dialysis event surveillance report for 2014. Clin J Am Soc Nephrol. 2017;12:1139–1146.
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004;39(3):309–17.
Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis. 2020;75(4):S1–164.
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, et al. Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;49(1):1–45.
Allon M, Brouwer-Maier DJ, Abreo K, Baskin KM, Bregel K, Chand DH, et al. Recommended Clinical Trial End Points for Dialysis Catheters. Clin J Am Soc Nephrol. 2018;13(3):495–500.
Kunin CM. Bennett and Brachman’s Hospital Infections. JAMA. 2008;300(11):1361–2.
Gominet M, Compain F, Beloin C, Lebeaux D. Central venous catheters and biofilms: where do we stand in 2017? APMIS. 2017;125(4):365–75.
Weiner LM, Webb AK, Limbago B, Dudeck MA, Patel J, Kallen AJ, et al. Antimicrobial-Resistant Pathogens Associated With Healthcare-Associated Infections: Summary of Data Reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Infect Control Hosp Epidemiol. 2016;37(11):1288–301.
Farrington CA, Allon M. Management of the Hemodialysis Patient with Catheter-Related Bloodstream Infection. Clin J Am Soc Nephrol. 2019;14(4):611–3.
Arora P, Obrador GT, Ruthazer R, Kausz AT, Meyer KB, Jenuleson CS, et al. Prevalence, Predictors, and Consequences of Late Nephrology Referral at a Tertiary Care Center. J Am Soc Nephrol. 1999;10(6),1281-6.
Wilson SM, Robertson JA, Chen G, Goel P, Benner DA, Krishnan M, et al. The IMPACT (Incident Management of Patients, Actions Centered on Treatment) program: a quality improvement approach for caring for patients initiating long-term hemodialysis. Am J Kidney Dis. 2012; 60(3):435–43.
Aitken E, Thomson P, Bainbridge L, Kasthuri R, Mohr B, Kingsmore D. A randomized controlled trial and cost-effectiveness analysis of early cannulation arteriovenous grafts versus tunneled central venous catheters in patients requiring urgent vascular access for hemodialysis. J Vasc Surg. 2017;65(3):766–74.
Raad II, Hohn DC, Gilbreath BJ, Suleiman N, Hill LA, Bruso PA, et al. Prevention of Central Venous Catheter-Related Infections by Using Maximal Sterile Barrier Precautions During Insertion. Infect Control Hosp Epidemiol. 1994;15(4):231–8.
Kosa SD, Gafni A, House AA, Lawrence J, Moist L, Nathoo B, et al. Hemodialysis Infection Prevention Protocols Ontario—Shower Technique (HIPPO-ST): A Pilot Randomized Trial. Kidney Int Rep. 2017;2(2):228–38.
O’Grady NP. Guidelines for the Prevention of Intravascular Catheter-Related Infections Clin infect dis. 2011;52(9):e126-93
Fisher M, Golestaneh L, Allon M, Abreo K, Mokrzycki MH. Prevention of Bloodstream Infections in Patients Undergoing Hemodialysis. Clin J Am Soc Nephrol. 2020;15(1):132–51.
Hymes JL, Mooney A, Van Zandt C, Lynch L, Ziebol R, Killion D. Dialysis Catheter-Related Bloodstream Infections: A Cluster-Randomized Trial of the ClearGuard HD Antimicrobial Barrier Cap. Am J Kidney Dis. 2017;69(2):220–7.
FDA issues warning on triCitrasol dialysis catheter anticoagulant [Internet]. [cited 2021 Jan 7]. Available from: http://www.m2.com/m2/web/story.php/2000A7C52BD5BF4A5240802568C4003B0B87
Hemmelgarn BR, Moist LM, Lok CE, Tonelli M, Manns BJ, Holden RM, et al. Prevention of Dialysis Catheter Malfunction with Recombinant Tissue Plasminogen Activator. N Engl J Med. 2011;364(4):303–12.
Mermel LA, Alang N. Adverse effects associated with ethanol catheter lock solutions: a systematic review. J Antimicrob Chemother. 2014;69(10):2611–9.
El-Hennawy AS, Frolova E, Romney WA. Sodium bicarbonate catheter lock solution reduces hemodialysis catheter loss due to catheter-related thrombosis and blood stream infection: an open-label clinical trial. Nephrol Dial Transplant. 2019;34(10):1739–45.
Piraino B. Staphylococcus aureus Prophylaxis in Dialysis Patients. Blood purif. 2000;18(4):350–4.
Gahlot R, Nigam C, Kumar V, Yadav G, Anupurba S. Catheter-related bloodstream infections. Int J Crit Illn Inj Sci. 2014;4(2):162–7.