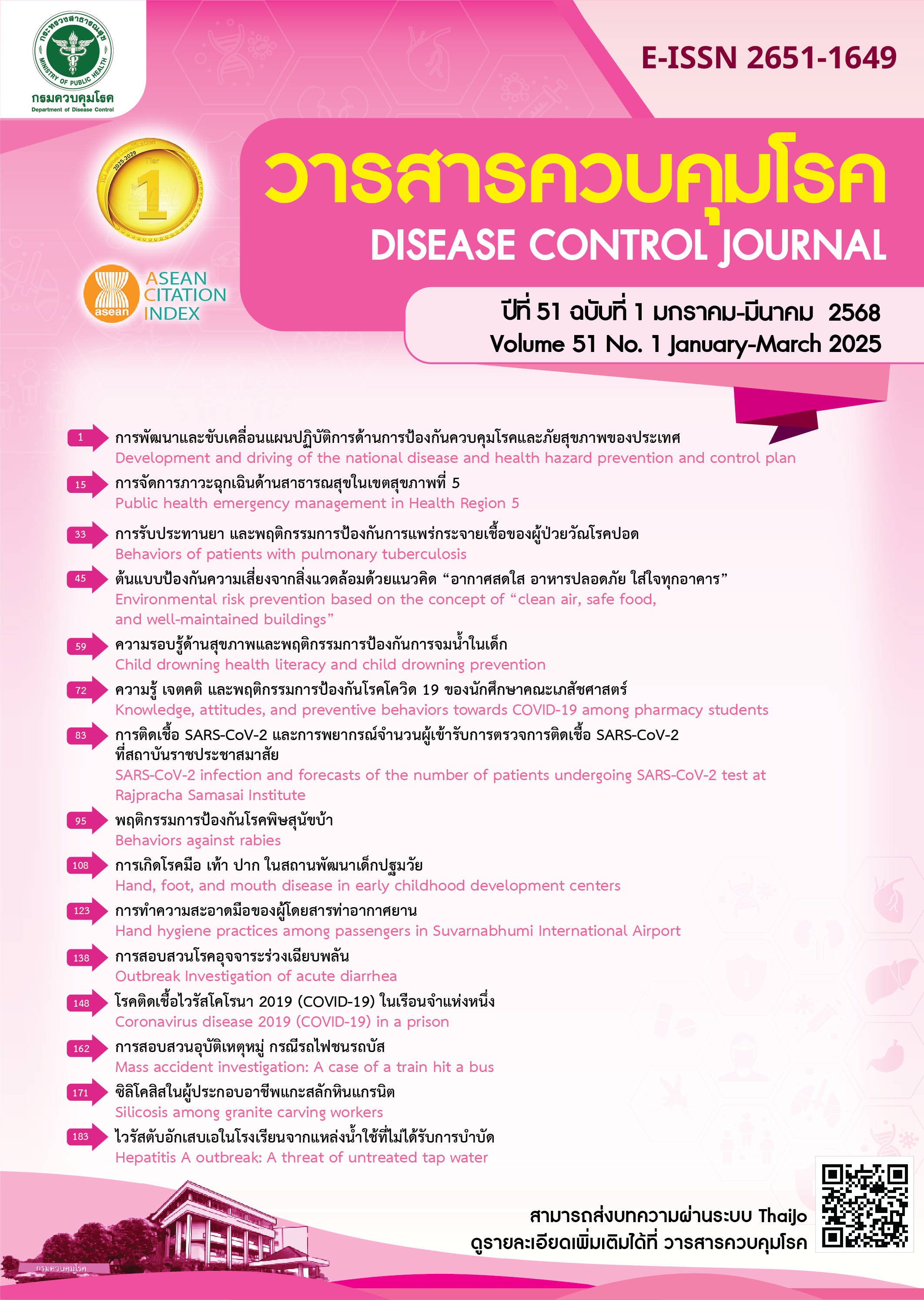
Situations and factors associated with SARS-CoV-2 infection during 2022-2024 and forecasts of the number of patients undergoing SARS-CoV-2 test at Rajpracha Samasai Institute during 2024-2025
DOI:
https://doi.org/10.14456/dcj.2025.7Keywords:
COVID-19, infection, risk factors, forecastingAbstract
Although the Thai Government has officially declared the end of the COVID-19 pandemic, Rajpracha Samasai Institute still detects cases of SARS-CoV-2 infection. This study aimed to (1) examine the number of individuals undertaking SARS-CoV-2 testing and individuals infected with COVID-19 at Rajpracha Samasai Institute from October 1, 2022, to May 31, 2024, (2) identify factors associated with SARS-CoV-2 detection, and (3) forecast the number of individuals seeking SARS-CoV-2 testing from June 1, 2024 to January 31, 2025. This study utilized a time-series cross-sectional dataset and analyzed data from 1,801 individuals using descriptive statistics. Binary logistic regression was applied to assess infection-related factors. Forecasting models including seasonal autoregressive integrated moving average (SARIMA), seasonal exponential smoothing (SES), and a 3-month moving average (3-MA) were conducted. The results showed that 28.2% of individuals tested positive for SARS-CoV-2 (42.8%, 24.9%, and 23.6% in 2022, 2023, and 2024, respectively). Being female, aged 18 years or older, having cough, and experiencing fever were significantly associated with a positive SARS-CoV-2 test result. Forecasting results indicated that the estimated number of individuals seeking testing would be approximately 90 and 70 per month based on the SES and 3-MA models, respectively. The SARIMA(0,0,0)(0,1,0)12 model predicted monthly variations ranging from 37 to 123 cases. Nonetheless, some limitations remained such as the absence of risk information from communities or immunity level, and the relatively short timeframe of the dataset used for forecasting. However, the findings can be useful for appropriate resource allocation and planning for SARS-CoV-2 testing services at Rajpracha Samasai Institute in the future.
Downloads
References
Pongpirul WA, Pongpirul K, Ratnarathon AC, Prasithsirikul W. Journey of a Thai Taxi Driver and Novel Coronavirus. N Engl J Med. 2020;382(11):1067-8.
Smith DR. Review a brief history of coronaviruses in Thailand. J Virol Methods. 2021;289:114034.
Sadarangani M, Abu Raya B, Conway JM, Iyaniwura SA, Falcao RC, Colijn C, et al. Importance of COVID-19 vaccine efficacy in older age groups. Vaccine. 2021;39(15):2020-3.
Biganzoli G, Mendola M, Perrone PM, Antonangeli LM, Longo ABE, Carrer P, et al. The Effectiveness of the Third Dose of COVID-19 Vaccine: When Should It Be Performed?. Vaccines. 2024;12(3):315.
Pairayayutakul N, Boontham S, Charanasri C, Promsart N. Vaccination and effectiveness of COVID-19 vaccine in real world in high-risk close contacts in Bangkok. Disease Control Journal [Internet]. 2022 Dec 30 [cited 2024 Nov 23];48(4):737-49. Available from: https://he01.tci-thaijo.org/index.php/DCJ/article/view/258056.
Nittayasoot N, Suphanchaimat R, Thammawijaya P, Jiraphongsa C, Siraprapasiri T, Ploddi K, et al. Real-World Effectiveness of COVID-19 Vaccines against Severe Outcomes during the Period of Omicron Predominance in Thailand: A Test-Negative Nationwide Case-Control Study. Vaccines (Basel). 2022;10(12):2123.
Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. International Journal of Infectious Diseases. 2022;114:252-60.
Pascarella G, Strumia A, Piliego C, Bruno F, Del Buono R, Costa F, et al. COVID-19 diagnosis and management: a comprehensive review. J Intern Med. 2020;288(2):192-206.
Pan F, Yang L, Li Y, Liang B, Li L, Ye T, et al. Factors associated with death outcome in patients with severe coronavirus disease-19 (COVID-19): a case-control study. Int J Med Sci. 2020;17(9):1281-92.
Wu C, Qian Y. The gender peak effect: Women are most vulnerable to infections during COVID-19 peaks. Front Public Health. 2022;10:937179.
Doerre A, Doblhammer G. The influence of gender on COVID-19 infections and mortality in Germany: Insights from age- and gender-specific modeling of contact rates, infections, and deaths in the early phase of the pandemic. PLoS One. 2022;17(5):e0268119.
Wenham C, Smith J, Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(10227):846-8.
Jegerlehner S, Suter-Riniker F, Jent P, Bittel P, Nagler M. Diagnostic accuracy of a SARS-CoV-2 rapid antigen test in real-life clinical settings. Int J Infect Dis. 2021;109:118-22.
Brihn A, Chang J, K OY, Balter S, Terashita D, Rubin Z, et al. Diagnostic Performance of an Antigen Test with RT-PCR for the Detection of SARS-CoV-2 in a Hospital Setting-Los Angeles County, California, June-August 2020. MMWR Morb Mortal Wkly Rep. 2021;70 (19):702-6.
Hyndman RJ, Athanasopoulos G. Forecasting: Principles and practice. 2nd ed. Melbourne: OTexts; 2018.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Disease Control Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles published in the Disease Control Journal are considered as academic work, research or analysis of the personal opinion of the authors, not the opinion of the Thailand Department of Disease Control or editorial team. The authors must be responsible for their articles.